Many people feel uneasy when they pick up their prescription and see a different pill than what they’re used to. The label says it’s the same medicine-but it’s cheaper, looks different, and has a different name. It’s natural to wonder: Is this generic drug really the same? You’re not alone. Thousands of patients every day ask the same questions. And the truth? Most of the fears around generics are based on myths, not science.
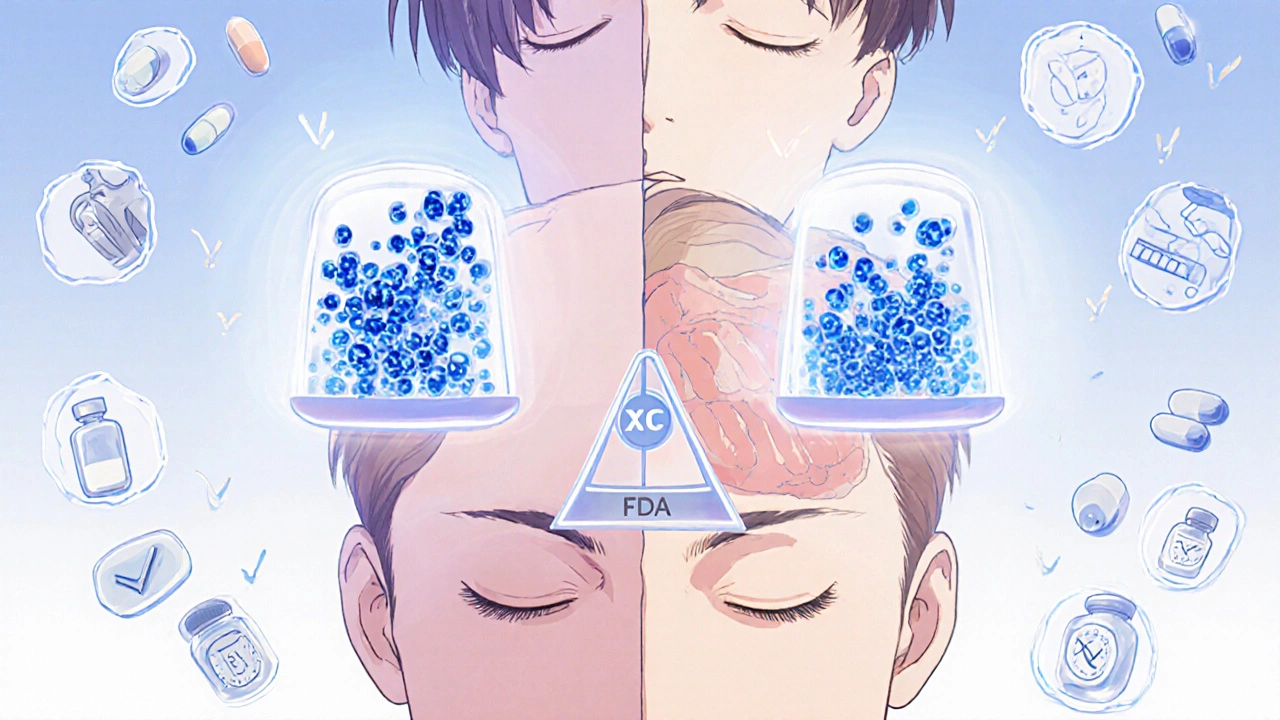
Are generic drugs really as effective as brand-name ones?
Yes. Every generic drug approved by the U.S. Food and Drug Administration (FDA) must contain the exact same active ingredient, in the same strength, and work the same way in your body as the brand-name version. That’s not a guess-it’s a legal requirement. Before a generic can hit the shelf, manufacturers must prove it’s bioequivalent. That means your body absorbs the medicine at the same rate and to the same extent as the brand-name drug. The FDA allows only a tiny range of difference-between 80% and 125%-in how much of the drug enters your bloodstream. That’s tighter than the variation you’d see between two batches of the same brand-name drug made months apart.
Think of it like this: two different brands of aspirin both contain acetylsalicylic acid. One might be white and round, another might be red and oval. But if you take one, your headache goes away the same way. Generics work the same way. Over 90% of all prescriptions filled in the U.S. are for generics-and they’re used in hospitals, clinics, and homes every day without issue.
Why do generic pills look different?
Because the law says they have to. Brand-name drug companies own the shape, color, and logo of their pills. Once a patent expires, other companies can make the same medicine-but they can’t copy the appearance. That’s why your generic metformin might be blue instead of white, or your generic lisinopril might be oval instead of round. The active ingredient? Identical. The fillers, dyes, or coatings? Those are different. But they don’t change how the drug works. They’re just there to hold the pill together or make it easier to swallow.
Some patients worry that a different color or shape means the medicine is weaker. That’s not true. A 2014 survey of 753 patients with chronic illnesses found that 87% believed generics were just as effective-even though many didn’t know why they looked different. The appearance change is purely cosmetic, not clinical.
Do generic drugs have more side effects?
No. Side effects come from the active ingredient, not the filler or color. If you had nausea with the brand-name version, you might get it with the generic too-but not because it’s generic. You might even notice side effects more when you switch, simply because you’re paying closer attention. That’s called the nocebo effect: expecting something to cause problems makes you more likely to notice them.
One common myth is that generics contain more chemicals to make them “stronger.” That’s not how it works. In fact, generics have to prove they’re just as safe, not stronger. A CDC study in rural communities found some patients believed generics had “more in it to make it stronger,” leading to dizziness or headaches. But there’s no evidence supporting that. The FDA requires all ingredients-active and inactive-to meet the same strict quality standards as brand-name drugs.
Could a generic drug be fake or contain no active ingredient?
No. That’s not possible with FDA-approved generics. Every batch of generic medicine is tested. The FDA inspects manufacturing sites-both in the U.S. and overseas-using the same standards as for brand-name drugs. In fact, about half of all generic medications are made by the same companies that make the brand-name versions. If you’re taking a generic, it might have been made in the same factory as the brand, just under a different label.
The FDA’s Risk Identification and Correction Action Program (RICA) has fixed over 1,200 potential quality issues since 2018. That’s not a sign of failure-it’s proof the system works. If something’s off, they catch it before it reaches patients.
Are generics cheaper because they’re lower quality?
Not at all. They’re cheaper because they don’t have to repeat expensive clinical trials. Brand-name companies spend billions developing a new drug-testing it in thousands of patients, running studies for years, and marketing it. Once the patent runs out, other companies can make the same drug. They only need to prove it behaves the same way in the body. That cuts development costs by 90%. Multiple manufacturers enter the market, and competition drives prices down.
The result? Generics save patients and the healthcare system billions. Over the past decade, generics saved the U.S. system $2.2 trillion. On average, each generic prescription saves $442 compared to the brand. That’s money you can put toward food, rent, or other meds.
When should I be cautious about switching to a generic?
There are a few exceptions. Some drugs have a very narrow therapeutic index-meaning the difference between a helpful dose and a harmful one is tiny. For these, even small changes in how the drug is absorbed can matter. Examples include:
- Warfarin (a blood thinner)
- Levothyroxine (for thyroid conditions)
- Phenytoin and levetiracetam (for seizures)
If you’re on one of these, your doctor may recommend staying on the same version-brand or generic-unless they specifically approve a switch. Even then, most patients switch safely. The key is monitoring. If you switch, your doctor might check your blood levels a few weeks later to make sure everything’s still on track.
But for the vast majority of medications-antibiotics, blood pressure pills, antidepressants, statins, diabetes drugs-switching to a generic is safe and effective. No extra monitoring is needed.
Why do some people still refuse generics?
It’s not just about science. It’s about trust. Many patients grew up hearing “name brands are better.” That message sticks. Cultural beliefs, personal experiences, and stories from friends can be powerful. A 2014 study found non-Caucasian patients were significantly more likely to ask for brand-name drugs-even when their doctors recommended generics. In rural areas, patients often heard from neighbors that generics “didn’t work as well.”
That’s why communication matters. Pharmacists can help explain the difference between appearance and effectiveness. Doctors can reassure patients that generics aren’t second-rate. Sometimes, just hearing, “I’ve prescribed this generic to hundreds of patients, and it works just as well,” makes all the difference.
Can I ask my doctor to prescribe only brand-name drugs?
Yes. You have the right to ask. But your doctor might ask why. If cost is the issue, they can help you find a generic that’s covered by your insurance. If you’re worried about effectiveness, they can explain the science. And if you’ve had a bad experience with a generic before, they’ll listen. Some doctors will write “Do Not Substitute” on the prescription. That means the pharmacist must give you the brand-name version-even if a generic is available.
But here’s the thing: most doctors don’t know every generic that comes on the market. They rely on pharmacists to help guide patients to the best, most affordable option. Pharmacists are trained to spot interactions, explain differences, and help you stay on your meds. That’s part of their job.
What should I do if I think the generic isn’t working?
Don’t stop taking it. Don’t assume it’s broken. Call your doctor or pharmacist. Sometimes, what feels like the drug isn’t working is actually your body adjusting. Or maybe your condition changed. Or maybe you’re taking it at the wrong time of day. Rarely, it’s the medicine. But if you’ve switched from brand to generic and feel worse, it’s worth checking in. Your provider might suggest switching back-or checking your blood levels, if it’s a drug like warfarin or levothyroxine.
Most of the time, though, the problem isn’t the generic. It’s the stress of change.
Bottom line: Generics are safe, effective, and save money
Generic drugs aren’t a compromise. They’re the same medicine, just without the brand-name markup. The FDA, doctors, pharmacists, and researchers all agree: for 99% of prescriptions, generics are just as good. The only difference is the price tag-and the peace of mind that comes from knowing you’re getting the same treatment without paying extra.
If you’re unsure about your prescription, ask. Ask your pharmacist. Ask your doctor. Ask questions. You deserve to understand what’s in your body-and you deserve to afford it.
Are generic drugs less effective than brand-name drugs?
No. Generic drugs must contain the same active ingredient, in the same strength and dosage form, and work the same way in your body as the brand-name version. The FDA requires proof of bioequivalence before approval, meaning the drug is absorbed into your bloodstream at the same rate and extent as the original. Over 90% of prescriptions in the U.S. are filled with generics, and they’re used safely every day in hospitals and homes.
Why do generic pills look different from brand-name ones?
By law, generic manufacturers can’t copy the appearance of brand-name pills, including color, shape, or logo. These differences are only cosmetic. The active ingredient and how it works in your body are identical. The change in appearance is meant to avoid trademark infringement, not to affect effectiveness or safety.
Do generic drugs cause more side effects?
No. Side effects come from the active ingredient, not the fillers or dyes used in the pill. If you experienced side effects with the brand-name version, you may experience them with the generic too-but not because it’s generic. Some people notice side effects more after switching due to psychological expectations, not actual changes in the drug’s effect.
Can I trust that a generic drug contains the right amount of medicine?
Yes. Every batch of generic medication is tested for quality, strength, and purity. The FDA inspects manufacturing facilities using the same standards as for brand-name drugs. About half of all generics are made by the same companies that produce the original brand-name versions. The FDA’s Risk Identification and Correction Action Program has resolved over 1,200 potential quality issues since 2018.
Are there any drugs I shouldn’t switch to generic?
For most medications, switching is safe. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, phenytoin, or levetiracetam-even small changes in absorption can matter. In these cases, your doctor may recommend staying on the same version (brand or generic) or monitoring your blood levels after a switch. Always talk to your provider before switching these types of drugs.




Christine Eslinger
November 17, 2025 AT 04:20