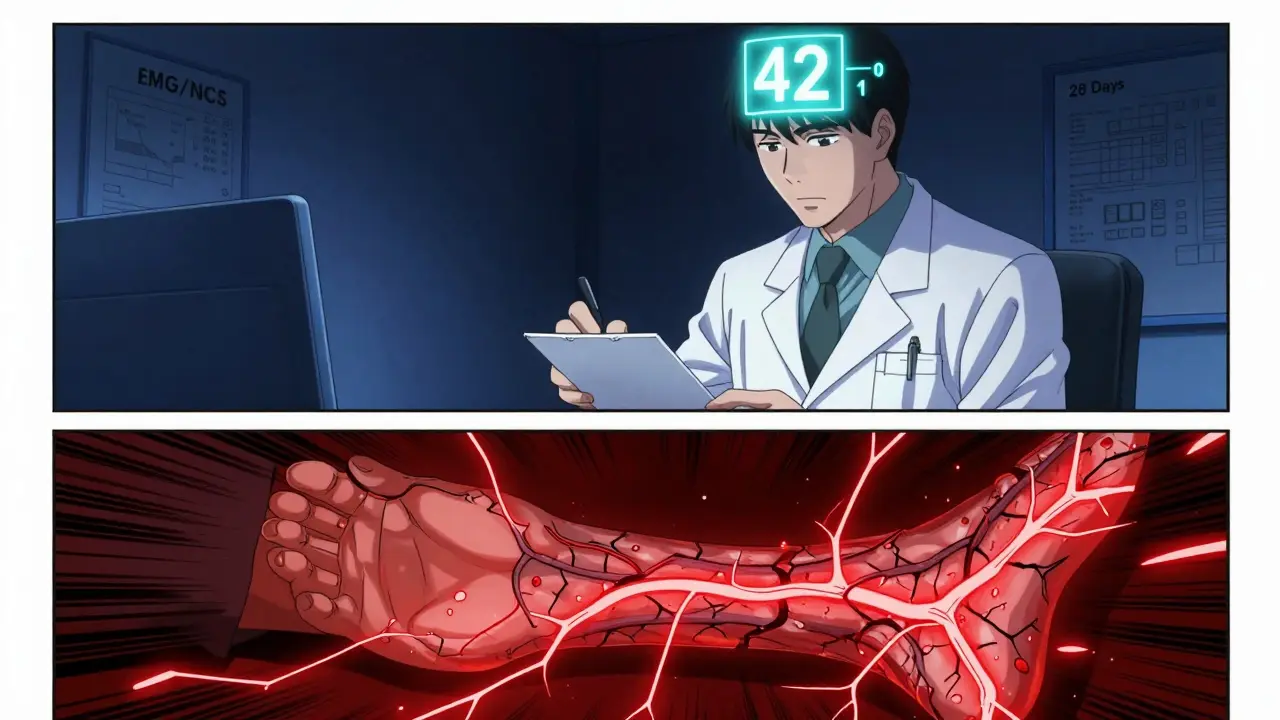
Metronidazole Neuropathy Risk Calculator
Track your metronidazole dose to understand your neuropathy risk. The article states that risks increase significantly after exceeding 42 grams cumulative dose.
What You Need to Know About Metronidazole and Numbness
It’s 2026, and millions of people still take metronidazole - sold under brand names like Flagyl - for infections like bacterial vaginosis, C. diff, or H. pylori. Most assume it’s safe because it’s cheap, common, and prescribed often. But if you’ve been on it for more than a few weeks and started feeling numbness, tingling, or burning in your hands or feet, you’re not imagining it. This isn’t just a side effect - it’s metronidazole neuropathy, a serious and often missed neurological injury.
How a Common Antibiotic Can Damage Your Nerves
Metronidazole was developed in the 1960s to kill anaerobic bacteria and parasites. It works by breaking down inside microbial cells and creating toxic compounds that destroy their DNA. But here’s the catch: it doesn’t stop there. Metronidazole crosses the blood-brain barrier and can also enter your peripheral nerves. Once there, its chemical structure gets reduced by nerve cells, creating free radicals that swell and damage nerve fibers. This isn’t a guess - it’s been proven in animal studies and confirmed in human nerve biopsies.
The damage starts subtly. You might notice a pins-and-needles feeling in your toes, or a strange warmth that doesn’t go away. It creeps up slowly, like a tide rising. Within weeks, the tingling spreads to your fingers. Walking becomes awkward. Nighttime is the worst - the burning gets worse when you’re lying still. Sleep disappears. That’s not just discomfort. That’s your sensory nerves dying.
The 42-Gram Threshold: When Risk Skyrockets
Not everyone who takes metronidazole gets neuropathy. But there’s a clear tipping point: 42 grams of cumulative dose. That’s 500mg three times a day for 28 days. Once you hit that mark, your risk of nerve damage jumps 10 times. A 2017 analysis of 13 studies found that 17.9% of patients who exceeded 42 grams developed neuropathy. Only 1.7% of those who stayed under it did.
Here’s what that looks like in real life:
- A 52-year-old man with a liver abscess takes metronidazole for 12 weeks - total dose: 168 grams. He starts feeling electric shocks in his fingers. He can’t grip tools anymore. His carpentry job ends.
- A 69-year-old woman with diverticulitis gets prescribed metronidazole for 10 weeks - total dose: 55 grams. Her feet burn constantly. She can’t wear socks. Gabapentin barely helps.
- A teenager on metronidazole for C. diff prophylaxis develops not just numbness, but temperature dysregulation - her feet feel like ice even in summer. She has to soak them in cold water to stop the pain.
These aren’t rare. They’re predictable. And they’re avoidable.
Why Doctors Miss It - And Why You Shouldn’t
Metronidazole neuropathy is misdiagnosed more often than you’d think. Patients with diabetes get told it’s diabetic neuropathy. Older adults get labeled with "age-related nerve wear." Some are even sent to psychiatrists because their symptoms don’t fit a textbook pattern.
The truth? Metronidazole neuropathy has a signature pattern: symmetric, distal, sensory-first. It starts in the feet, climbs up the legs, then moves to the hands. Motor weakness comes later - if at all. And unlike diabetic neuropathy, it often comes with severe nighttime pain and autonomic symptoms like abnormal sweating or temperature sensitivity.
And here’s the kicker: many doctors still don’t know about the 42-gram threshold. A 2023 survey found only 38% of primary care physicians could identify it. If your doctor didn’t warn you about this, it’s not your fault. It’s a systemic gap in medical education.
What to Do If You’re Already Experiencing Symptoms
If you’re on metronidazole and feel numbness, tingling, or burning - stop. Immediately. Don’t wait for a test. Don’t wait for your next appointment. Don’t assume it’s "just a side effect."
Here’s what happens next:
- Stop the drug. This is the single most important step. Recovery starts the moment you quit.
- See a neurologist. Ask for an EMG/NCS (electromyography and nerve conduction study). This confirms axonal damage - the hallmark of metronidazole toxicity.
- Start physical therapy. Studies show patients who get structured rehab recover 37% faster. Balance training, sensory re-education, and gentle strengthening help rewire damaged nerves.
- Track your recovery. Improvement can take weeks to months. Some feel better in 2 weeks. Others take 6 months. Patience matters. But so does persistence.
Recovery isn’t guaranteed - but it’s likely. In 94% of cases, symptoms improve or vanish after stopping the drug. Only 6% develop permanent damage. That’s why acting fast is non-negotiable.
What’s Being Done to Prevent This?
Things are changing. Mayo Clinic now blocks electronic prescriptions for metronidazole beyond 28 days unless an infectious disease specialist approves it. The FDA updated the drug label in 2023 to highlight the 42-gram threshold. The Infectious Diseases Society of America now recommends avoiding metronidazole beyond that dose unless absolutely necessary.
Research is moving forward too. A clinical trial at UCSF is testing whether alpha-lipoic acid - a common antioxidant supplement - can protect nerves when taken alongside metronidazole. Early results are promising. If proven, this could become a standard protective strategy for patients needing long-term therapy.
But until then, the best protection is awareness. If you’re prescribed metronidazole for more than 14 days, ask: "What’s the total dose? Is there a safer alternative?" If you’re already past 42 grams and have symptoms - act now.

When to Worry - And When to Breathe
Short courses? 5 to 7 days for bacterial vaginosis or giardiasis? The risk of neuropathy is near zero. The side effects you might feel - metallic taste, nausea, dizziness - are annoying but harmless.
Long courses? 3 weeks or more? Especially if you’re over 60, diabetic, or have kidney issues? Now you’re in the danger zone. Keep a symptom journal. Note when the tingling started, where it is, and whether it’s getting worse.
And if you’ve been on metronidazole for more than 28 days and feel anything unusual in your hands or feet - don’t wait. Don’t hope it goes away. This isn’t something you can outwait.
Alternatives to Metronidazole
There are other options. For bacterial vaginosis, clindamycin cream or vaginal probiotics work well. For H. pylori, newer triple therapies use amoxicillin and clarithromycin instead. For C. diff, fidaxomicin has a lower neurotoxic risk than metronidazole - though it’s more expensive.
Cost matters. But permanent nerve damage costs more. A 2022 Duke University study found each case of lasting metronidazole neuropathy adds $247,000 in lifetime healthcare costs - from pain meds to physical therapy to lost wages. Preventing it saves money, too.
Final Word: Don’t Assume Safety
Metronidazole is not dangerous because it’s a bad drug. It’s dangerous because we treat it like it’s harmless. We forget it’s a potent chemical that can cross into your nerves. We forget that "common" doesn’t mean "safe for long-term use."
If you’re reading this because you’ve felt tingling in your toes - you’re not alone. And you’re not crazy. You’re one of the many who’ve been silently injured by a drug we thought we understood.
Stop it. Get checked. Tell your doctor. And if they don’t know about the 42-gram threshold? Show them. This isn’t just about your feet. It’s about your body’s right to be protected - even when the medicine is supposed to heal you.






Marc Bains
January 31, 2026 AT 09:07