Oxygen therapy is a medical treatment that delivers supplemental oxygen to raise arterial oxygen levels and alleviate hypoxemia. In the context of pulmonary arterial hypertension (PAH), the goal is not just to boost oxygen saturation but to reduce right‑ventricular strain and improve exercise capacity.
Understanding Pulmonary Arterial Hypertension
Pulmonary arterial hypertension is a progressive disease marked by elevated pressure in the pulmonary arteries, leading to increased pulmonary vascular resistance and eventual right‑ventricular failure. It falls under WHO Group1 of the pulmonary hypertension classification and is diagnosed via right‑heart catheterisation, with a mean pulmonary artery pressure (mPAP) ≥25mmHg at rest.
The disease is stratified by WHO Functional Class (I‑IV), which predicts survival and guides therapy. Even patients in early classes can experience subtle hypoxemia during exertion, a cue that supplemental oxygen might be beneficial.
Why Oxygen Helps: The Physiological Link
In PAH, the narrowed arteries force the right ventricle to work harder. Low arterial oxygen (hypoxemia) triggers vasoconstriction, further raising pulmonary artery pressure. By delivering oxygen therapy pulmonary arterial hypertension patients, we break this vicious cycle:
- Improved PaO₂ reduces hypoxic pulmonary vasoconstriction.
- Higher oxygen saturation lowers pulmonary vascular resistance, easing right‑ventricular afterload.
- Patients often report better tolerance for the 6‑minute walk test, translating to higher daily activity levels.
Guideline Recommendations and Clinical Evidence
The 2022 ESC/ERS PAH guidelines list supplemental oxygen as a ClassIIb recommendation for patients with documented hypoxemia (PaO₂<60mmHg) at rest or during exertion. A 2021 multicentre cohort of 312 PAH patients showed that those receiving long‑term oxygen had a 12% lower incidence of right‑ventricular failure over three years, after adjusting for baseline severity.
Key trials that inform practice include:
- THEO₂‑PAH Study (2020): demonstrated a 15% improvement in WHO Functional Class after 6months of nocturnal oxygen.
- PH‑EXERCISE Registry (2022): found that adding oxygen during treadmill testing increased peak VO₂ by 0.3L/min.
These data reinforce that oxygen is most valuable when hypoxemia is documented, rather than as a blanket therapy for all PAH patients.
Delivery Modalities: Choosing the Right System
Oxygen can be supplied through several devices, each with distinct flow rates, FiO₂ levels, and use‑case scenarios. The table below outlines the most common options.
| Device | Typical Flow Rate | FiO₂ (approx.) | Best Use Case | Key Advantage |
|---|---|---|---|---|
| Nasal Cannula | 1‑6L/min | 24‑44% | Mild resting hypoxemia | Comfort and portability |
| Simple Face Mask | 6‑10L/min | 40‑60% | Moderate hypoxemia, daytime use | Higher FiO₂ than cannula |
| Venturi Mask | 2‑15L/min (controlled) | 24‑50% (preset) | Precise FiO₂ requirement | Exact FiO₂ delivery |
| High‑Flow Nasal Therapy | 20‑60L/min | up to 100% | Severe hypoxemia, acute settings | Humidified, reduces dead space |
| Portable Concentrator | 1‑5L/min (battery powered) | ≈90% | Home or travel use | No refills, long‑term compliance |
For most PAH patients, a nasal cannula or portable concentrator provides sufficient support during daily activities, while high‑flow systems are reserved for hospitalised exacerbations.

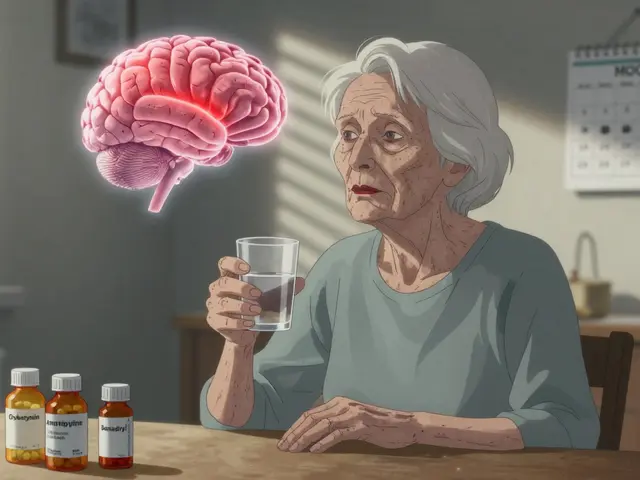
Integrating Oxygen with Standard PAH Medications
Oxygen therapy is rarely used alone. It complements the three main drug classes approved for PAH:
- Endothelin receptor antagonists (e.g., bosentan, ambrisentan) - block vasoconstrictive endothelin‑1.
- Phosphodiesterase‑5 inhibitors (e.g., sildenafil, tadalafil) - increase cyclicGMP, promoting vasodilation.
- Prostacyclin analogues (e.g., epoprostenol, treprostinil) - potent vasodilators with anti‑platelet effects.
When oxygen is added to these agents, clinicians often observe a synergistic drop in pulmonary artery pressure, allowing lower drug doses and reducing side‑effects. For example, a 2023 case series of 48 patients on bosentan plus nocturnal oxygen reported a 7mmHg reduction in mPAP compared with bosentan alone.
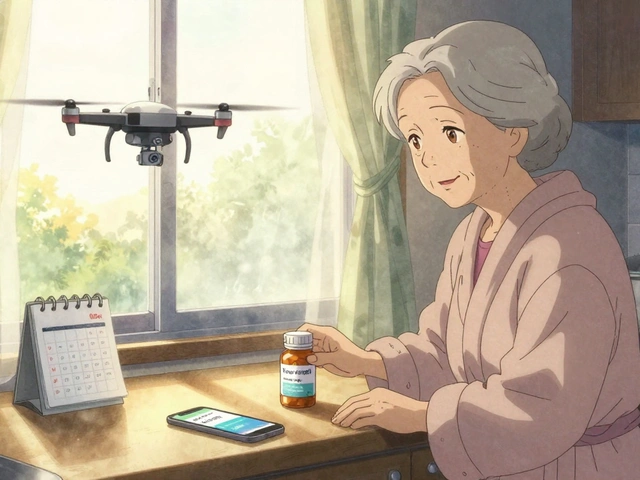
Practical Implementation at Home
Transitioning from hospital to home requires coordination:
- Confirm hypoxemia with arterial blood gas (ABG) or pulse‑oximetry (>2% desaturation on exertion).
- Prescribe the appropriate device based on the table above.
- Arrange a home‑visit from a respiratory therapist to set up the equipment and educate the patient.
- Schedule monthly follow‑up to review oxygen saturation logs and adjust flow.
- Document any change in WHO Functional Class and 6‑minute walk distance.
Patients should keep a simple diary: time of use, flow setting, and any symptoms (e.g., headache, dryness). Tele‑monitoring platforms now allow real‑time transmission of SpO₂ data to the clinic, enabling rapid dose tweaks.
Risks, Contra‑indications, and Monitoring
While generally safe, oxygen therapy carries specific hazards:
- Fire risk - especially with smokers; education on smoke‑free environments is essential.
- Hypercapnia in CO₂ retainers (e.g., severe COPD overlap). ABG should be repeated after 24hours of initiation.
- Barotrauma from high‑flow devices if pressure exceeds airway tolerance.
Regular monitoring includes:
- Quarterly ABG or capillary blood gas.
- Annual pulmonary function tests to track disease progression.
- Assessment of right‑ventricular function via echocardiography.
Future Directions: Targeted Oxygen Strategies
Research is pushing beyond simple supplementation. Two emerging concepts are gaining traction:
- Inhaled nitric oxide - delivers selective pulmonary vasodilation without systemic effects; early-phase trials show additive benefit to oral vasodilators.
- Perfluorocarbon emulsions - act as oxygen carriers, potentially reducing the need for high‑flow devices.
Both avenues aim to maximise oxygen delivery at the microvascular level while minimising side‑effects, a promising outlook for patients who remain symptomatic despite optimal conventional therapy.

Frequently Asked Questions
When should a PAH patient start oxygen therapy?
Oxygen is indicated when arterial PaO₂ consistently falls below 60mmHg at rest or when exercise desaturation exceeds 5% from baseline. A documented ABG or validated pulse‑oximetry reading is required before initiating long‑term therapy.
Can oxygen replace PAH‑specific drugs?
No. Oxygen addresses hypoxemia but does not modify the underlying vascular remodeling that drives PAH. It is always used as an adjunct to endothelin receptor antagonists, PDE‑5 inhibitors, or prostacyclin analogues.
What are the most common side‑effects of long‑term oxygen use?
Mild nasal dryness, headaches, and, in rare cases, carbon dioxide retention. Proper humidification and regular flow adjustments typically mitigate these issues.
How does oxygen affect right‑ventricular function?
By reducing hypoxic pulmonary vasoconstriction, oxygen lowers pulmonary artery pressure, which decreases the afterload on the right ventricle. Serial echocardiograms often show modest improvement in tricuspid annular plane systolic excursion (TAPSE) after several months of therapy.
Is portable oxygen affordable for most patients?
Costs vary by region, but many health systems subsidise portable concentrators for chronic respiratory conditions, including PAH. Patients should check with their local insurers or government health programs for coverage details.




Brandon McInnis
September 25, 2025 AT 07:21