Pentosan Polysulfate Treatment Timeline Simulator
How this tool works
This simulator estimates symptom improvement based on clinical data. It shows expected symptom scores at different treatment intervals, helping you understand the typical timeline for benefits with Pentosan Polysulfate. Note: Individual results may vary.
Results
Note: This simulation is based on clinical data showing average improvement. Individual results may vary. Symptoms typically improve most significantly after 6-12 months of treatment.
When you’ve tried everything for chronic pelvic pain and still feel the burn, you start wondering if there’s a hidden solution. Pentosan polysulfate is a prescription drug that has been used for decades to protect the bladder’s inner lining. It’s marketed under the brand name Elmiron in the United States and Cystaderm in Europe, and it’s the only oral therapy officially approved for Bladder Pain Syndrome (BPS). Below we break down why doctors prescribe it, how it actually helps, the latest research, and practical tips for anyone considering it.
Key Takeaways
- Pentosan polysulfate aims to restore the bladder’s glycosaminoglycan (GAG) layer, reducing irritation.
- Clinical trials show modest symptom improvement in 40‑60% of patients.
- Typical dose is 100 mg taken orally three times a day for at least six months.
- Common side effects include mild GI upset and rare pigment‑retinal changes.
- It works best when combined with lifestyle changes and other bladder‑friendly therapies.
What Is Bladder Pain Syndrome?
Bladder Pain Syndrome (BPS) refers to chronic pelvic pain, pressure, or burning that originates from the bladder and persists for at least six weeks. In many regions it’s called Interstitial cystitis (IC), though some clinicians use BPS as the broader term to encompass patients without classic cystoscopic findings. The hallmark is a fragile bladder lining that lets irritants leak into the muscle, causing inflammation and pain.
Key signs include:
- Frequent urination (often >8 times a day)
- Urgency without infection
- Pain that worsens as the bladder fills
- Pain that may radiate to the lower back, hips, or genitals
Because the cause isn’t fully understood, treatment focuses on symptom relief and protecting the bladder wall.
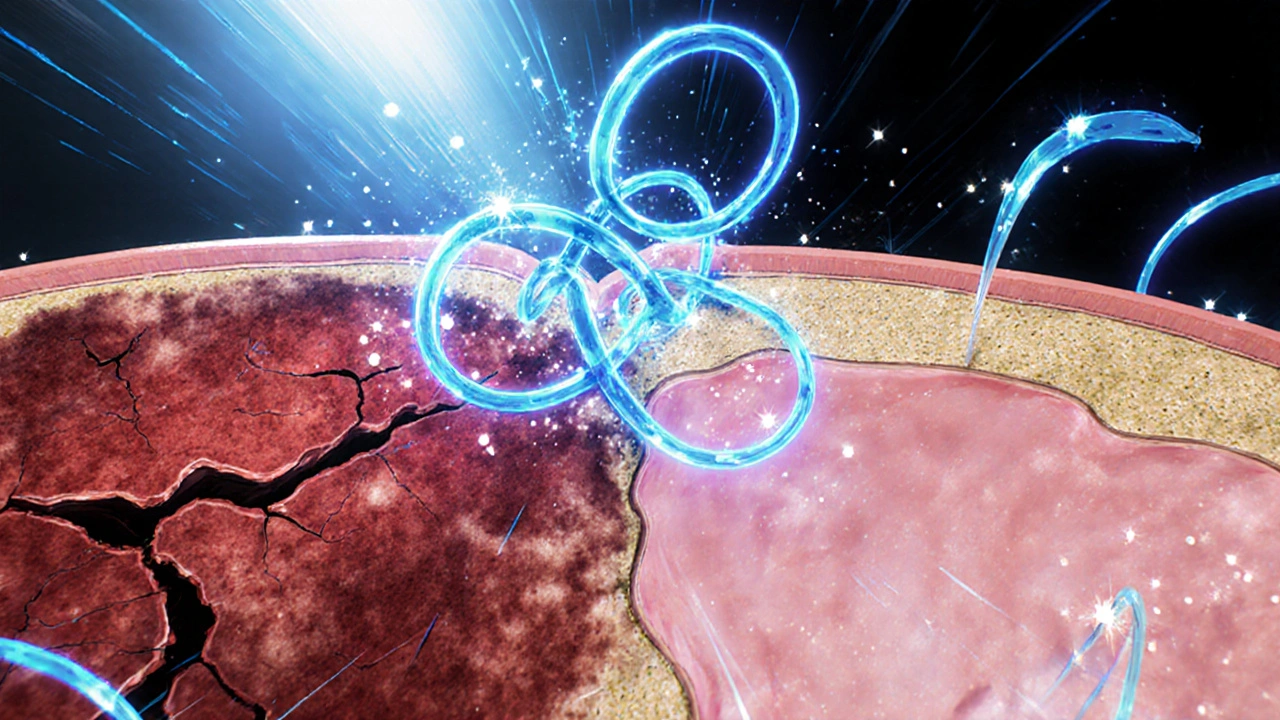
How Pentosan Polysulfate Works
The drug is a sulfated polysaccharide that mimics the natural GAG molecules lining the bladder. Think of the GAG layer as a waterproof coat; when it’s thin or missing, urine acids and toxins directly irritate the bladder muscle. Pentosan polysulfate binds to the urothelium, stimulating the production of new GAGs and helping seal the barrier.
Research from the FDA and the European Medicines Agency suggests three main actions:
- Restoration of the GAG coating
- Anti‑inflammatory effect via inhibition of cytokine release
- Potential anti‑angiogenic activity that reduces abnormal bladder blood vessel growth
These mechanisms together lower bladder hypersensitivity and, over time, can lessen urgency and pain.
Clinical Evidence: What the Numbers Say
Since its approval in the 1990s, dozens of randomized controlled trials (RCTs) and observational studies have evaluated pentosan polysulfate. A 2023 meta‑analysis of 12 RCTs (over 2,300 participants) reported:
- Mean reduction in symptom scores of 2.3 points on the O'Leary‑Sant Scale (scale 0‑12) compared with placebo.
- Responder rates (≥30% improvement) of 45% for the drug versus 22% for placebo.
- Benefit plateaued after about 6‑12 months, suggesting a minimum treatment window.
Real‑world registries from the US and Europe echo these findings, noting that patients who combine the medication with pelvic floor physical therapy see the highest gains.
Dosage, Administration, and Monitoring
Standard dosing is 100 mg taken orally three times daily (total 300 mg per day). Capsules should be swallowed whole with water; crushing may diminish the protective coating.
Because the drug can take months to show effect, clinicians usually schedule follow‑up visits at 3, 6, and 12 months to assess symptom scores, urine analysis, and, importantly, eye health. Recent reports link long‑term use (≥2 years) to pigmentary retinopathy, prompting the FDA to issue a warning in 2023. Patients over 50 or those with pre‑existing eye disease should have baseline retinal imaging and annual checks.
If a patient experiences GI upset, the dose can be split into four smaller doses or taken with food. In cases of severe side effects, tapering off rather than abrupt stopping helps avoid rebound bladder irritation.
Side Effects, Contraindications, and Safety Concerns
Overall, pentosan polysulfate is well‑tolerated. Common adverse events (≥5% of users) include:
- Mild nausea or stomach cramping
- Transient diarrhea
Rare but serious issues:
- Pigmentary retinopathy (vision changes, typically after >2 years)
- Allergic skin reactions
Contra‑indications are limited but include:
- Known hypersensitivity to the drug
- Severe renal impairment (eGFR <30 mL/min/1.73 m²)
Pregnancy and lactation are not well studied; most guidelines advise avoiding use unless benefits clearly outweigh risks.

Comparing Treatment Options for BPS
| Therapy | Mechanism | Typical Dose / Regimen | Evidence Strength | Common Side Effects |
|---|---|---|---|---|
| Pentosan polysulfate | GAG‑layer restoration, anti‑inflammatory | 100 mg PO TID | Moderate (meta‑analysis, RCTs) | Nausea, rare retinal changes |
| Amitriptyline (oral) | Tricyclic antidepressant, analgesic | 10‑25 mg PO daily | Low‑moderate (small RCTs) | Dry mouth, drowsiness |
| Hydroxyzine | Antihistamine, smooth‑muscle relaxant | 25‑50 mg PO BID | Low (observational) | Sedation, anticholinergic effects |
| Bladder hydrodistension (procedure) | Mechanical stretching of bladder wall | One‑time office procedure | Low‑moderate (case series) | Transient hematuria, infection risk |
| DMSO (intravesical) | Anti‑inflammatory, analgesic | 50 mL 50% solution retained 15 min | Low (small trials) | Garlic‑like breath, bladder irritation |
Choosing the right plan hinges on symptom severity, patient preferences, and potential drug interactions. Many urologists start with lifestyle tweaks-fluid management, bladder training, and pelvic floor physiotherapy-then add oral therapy. If pain persists after three months, stepping up to pentosan polysulfate or a combination regimen is common.
Practical Tips for Patients on Pentosan Polysulfate
- Set realistic expectations: Noticeable relief often takes 3‑6 months.
- Track symptoms: Use a simple diary or a validated questionnaire like the O'Leary‑Sant Scale.
- Stay hydrated, but avoid irritants: Limit caffeine, alcohol, citrus juices, and artificial sweeteners.
- Combine with pelvic‑floor therapy: Physical therapists can teach relaxation and trigger‑point release.
- Schedule eye exams: Baseline retinal imaging and yearly follow‑ups are essential.
- Discuss all meds with your doctor: Anticoagulants, NSAIDs, or other bladder‑active drugs may need adjustment.
Sometimes, insurance coverage can be tricky. In Australia, the PBS lists pentosan polysulfate for “chronic interstitial cystitis,” so patients should use the exact diagnostic code when filing a claim.
Frequently Asked Questions
How long does it take to feel better?
Most people notice a modest drop in urgency and pain after about 12 weeks, but the full benefit often requires 6‑12 months of consistent use.
Can I take pentosan polysulfate with other bladder meds?
Yes, it’s frequently combined with low‑dose amitriptyline or hydroxyzine. Your urologist should review all prescriptions to avoid duplicate side‑effects.
What should I do if I develop vision changes?
Stop the medication immediately and schedule an urgent retinal exam. Early detection can prevent permanent damage.
Is pentosan polysulfate safe during pregnancy?
There’s insufficient data, so clinicians usually advise against use unless the benefits clearly outweigh the unknown risks.
Do I need to take the drug forever?
Many patients stay on it long‑term because symptoms can flare when the drug stops. If you achieve stable control, your doctor may try a gradual taper and monitor for recurrence.
Bottom line: pentosan polysulfate isn’t a miracle cure, but for a sizeable slice of BPS sufferers it offers a biologically‑targeted way to repair the bladder’s protective shield. Pair it with diet tweaks, pelvic‑floor exercises, and regular eye checks, and you’ll have the best shot at reclaiming a comfortable life.




Abhishek Kumar
October 23, 2025 AT 18:40