Proctitis Food Trigger Checker
How This Tool Works
Select foods you commonly consume. The tool will assess your potential risk of triggering proctitis inflammation based on the latest research. After checking, you'll receive personalized insights and dietary recommendations.
Select Foods You Eat Regularly
Trigger Risk Assessment
Recommended Actions
Ever wonder why a simple bite of cheese or a bowl of wheat pasta could make your rectum feel raw? That uncomfortable burn often points to Proctitis, and for many people the culprit is hidden in the foods they love. This guide walks you through what proctitis is, how food allergies can spark it, and what you can do right now to feel better.
Understanding Proctitis
When you hear Proctitis is a inflammation of the lining of the rectum, you might picture an infection or a flare‑up of ulcerative colitis. In reality, proctitis is a localized form of inflammatory bowel disease (IBD) that concentrates in the last few centimeters of the colon. Typical symptoms include rectal pain, bleeding, mucus discharge, and a persistent urge to go even when the bowel is empty.
Doctors often diagnose it with a combination of a digital rectal exam, a flexible sigmoidoscopy, and a biopsy. The tissue sample helps distinguish plain proctitis from more specific sub‑types such as eosinophilic proctitis or ulcerative colitis involving the rectum.
Food Allergies 101
Food Allergies are immune‑mediated reactions that occur when the body mistakenly identifies a food protein as harmful. Unlike food intolerances, which are often digestive, true allergies trigger the release of histamine and other inflammatory chemicals from mast cells.
Common allergens include gluten, dairy (lactose and casein), nuts, shellfish, and certain fruits. When an allergic reaction hits the gut, it can cause swelling, increased mucus, and even microscopic ulcers-all of which can aggravate an already sensitive rectal lining.
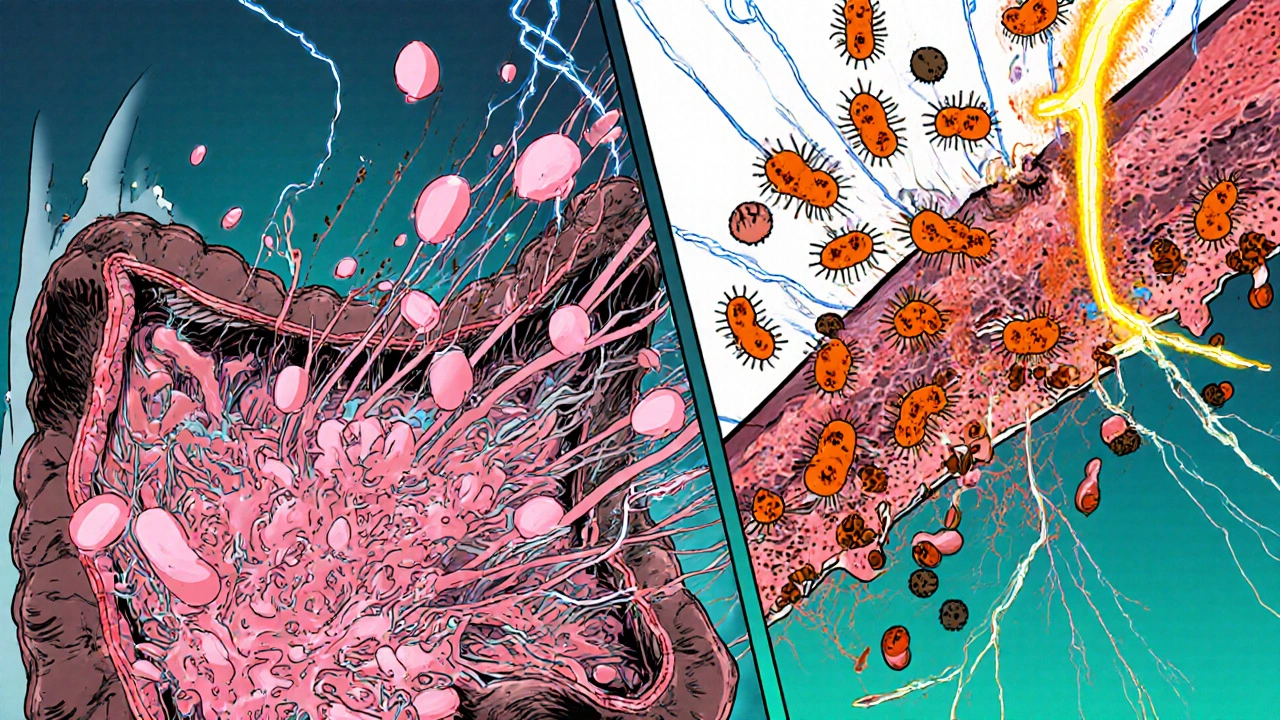
How Allergies Can Trigger Proctitis
Several mechanisms link food allergies to proctitis:
- Histamine surge: Histamine raises vascular permeability, making the rectal tissue more prone to bleeding and pain.
- Eosinophilic infiltration: In allergic individuals, eosinophils (a type of white blood cell) migrate to the gut and release toxic proteins that damage the mucosa.
- Gut‑brain axis: Food‑induced inflammation can alter nerve signaling, heightening the sensation of urgency.
- Microbiome disruption: Allergic reactions often shift the balance of gut bacteria, promoting species that produce irritating metabolites.
Research from the 2023 International Gastroenterology Forum showed that 22 % of patients with chronic proctitis also tested positive for specific IgE antibodies to wheat or dairy, suggesting a direct allergic component.
Identifying Your Dietary Triggers
Pinpointing the exact food that fuels your proctitis can feel like detective work, but a systematic approach makes it doable.
- Start a food‑symptom diary: Record everything you eat and any rectal symptoms for at least two weeks.
- Consider common allergens: Begin by eliminating gluten, lactose, and high‑FODMAP foods such as onions, garlic, and apples.
- Perform an elimination‑reintroduction protocol: After 2-4 weeks of strict avoidance, re‑introduce one food at a time every 3-4 days while monitoring symptoms.
- Get tested if needed: Serum specific IgE or skin‑prick tests can confirm suspected allergies, especially for nuts and shellfish.
For patients with eosinophilic proctitis, a biopsy will often reveal >20 eosinophils per high‑power field, which strongly points toward an allergic trigger.
Managing Symptoms Through Diet
The goal is to reduce inflammation while still getting balanced nutrition. Here are practical steps:
- Low‑FODMAP diet: Limits fermentable carbs that feed gas‑producing bacteria, easing rectal pressure.
- Gluten‑free regimen: Swap wheat, barley, and rye for rice, quinoa, and buckwheat.
- Lactose‑free alternatives: Use almond, oat, or coconut milk; choose aged cheeses that have lower lactose.
- Anti‑histamine foods: Incorporate vitamin C‑rich fruits (kiwi, strawberries) and omega‑3‑rich fish to blunt histamine release.
- Probiotic support: Strains like Lactobacillus rhamnosus GG and Bifidobacterium infantis have shown benefit in reducing gut inflammation.
Remember, sudden, extreme restrictions can lead to nutrient gaps. Working with a dietitian familiar with IBD ensures you stay well‑balanced.
Medical Treatments and When to Seek Help
Diet alone may not resolve severe inflammation. Conventional therapies include:
- Corticosteroid suppositories (e.g., hydrocortisone) for short‑term flare control.
- 5‑ASA (mesalamine) enemas that target the rectal lining directly.
- Oral antihistamines (cetirizine, loratadine) if a clear allergic pathway is identified.
- Biologic agents (infliximab, vedolizumab) for refractory cases linked to broader IBD.
If you experience heavy bleeding, unexplained weight loss, or fevers, schedule an urgent endoscopic evaluation. Early detection prevents complications like strictures or fistulas.
Quick Checklist for Proctitis Patients
- Track foods and symptoms daily.
- Eliminate gluten, lactose, and high‑FODMAP items for at least 4 weeks.
- Consider allergy testing if symptoms persist.
- Maintain a balanced intake of protein, healthy fats, and fiber.
- Use prescribed rectal meds as directed.
- Follow up with your gastroenterologist every 3-6 months.
Comparison: Typical Proctitis vs. Allergy‑Related Proctitis
| Aspect | Typical Proctitis (IBD‑related) | Allergy‑Related Proctitis |
|---|---|---|
| Primary trigger | Immune dysregulation, genetic factors | Specific food allergens (gluten, dairy, nuts) |
| Histology | Crypt distortion, neutrophils | Elevated eosinophils, mast cell degranulation |
| Response to diet | Limited; often requires medication | Often improves with elimination diet |
| Common symptoms | Bleeding, urgency, tenesmus | Same plus occasional hives or facial swelling |
| Diagnostic clues | Positive pANCA, colonoscopy findings | Positive specific IgE, eosinophilic infiltrate on biopsy |
Frequently Asked Questions
Can I eat any dairy if I have proctitis?
Most people with proctitis tolerate hard cheeses because the lactose content is low, but soft dairy and milk can still provoke histamine release. A short lactose‑free trial helps you decide.
Is a colonoscopy necessary for diagnosis?
A flexible sigmoidoscopy is usually sufficient since proctitis stays within the distal 15 cm. Colonoscopy is reserved for suspected extensive IBD.
Do antihistamines cure proctitis?
They can reduce inflammation if a food allergy is the main driver, but they won’t replace anti‑inflammatory meds needed for IBD‑related disease.
How long does an elimination diet take to show results?
Most patients notice a reduction in rectal urgency and bleeding within 2-4 weeks of strict avoidance.
Are probiotics safe for anyone with proctitis?
Yes, especially strains that support mucosal healing. However, immunocompromised patients should consult a doctor first.






Albert Fernàndez Chacón
October 18, 2025 AT 15:16