Every year, Australians fill over 200 million prescriptions. Most of them? Generic drugs. And behind that number is the Pharmaceutical Benefits Scheme - a system that keeps medicines affordable for millions, but also shapes how drugs are priced, approved, and used across the country. If you’ve ever paid $7.70 for a month’s supply of blood pressure pills, or waited months for a new cancer drug to be listed, you’ve felt the PBS in action.
What the PBS Actually Does
The Pharmaceutical Benefits Scheme (PBS) isn’t just a subsidy program. It’s Australia’s main tool for controlling drug prices and making sure everyone - whether they’re on a pension, working full-time, or just got laid off - can get the medicines they need. Since 1948, the government has paid for most of the cost of listed drugs. Patients pay a co-payment, and the rest? Covered by taxpayers. As of 2025, the PBS covers over 5,400 medicines. That’s not just pills - it includes inhalers, injections, patches, even some rare disease treatments. About 87% of all prescriptions dispensed in Australia are subsidized by the PBS. That means if you walk into a pharmacy with a valid Medicare card, you’re likely getting a drug that’s been negotiated down by the government. The key players? The Pharmaceutical Benefits Pricing Authority (PBPA) negotiates prices with drug makers. The Pharmaceutical Benefits Advisory Committee (PBAC) decides which drugs get listed based on how well they work and whether they’re worth the cost. Their main metric? Cost per quality-adjusted life year (QALY). The unofficial threshold? Around AU$50,000. That means if a drug costs more than $50,000 to give one extra year of healthy life, it’s usually a hard sell - unless it’s for a rare disease.How Generic Drugs Fit In
Australia’s generic drug market is huge. In 2024, generics made up 46% of total PBS spending - that’s $6.2 billion. But here’s the twist: generics account for 84% of all prescriptions by volume, but only 22% of the total value. Why? Because the price difference between brand-name and generic drugs is massive. Take a common statin like atorvastatin. When the patent expired, the original brand sold for about $35 per script. Within a year, five generic versions hit the market. The price dropped to $6.20. That’s an 82% drop. That’s the power of competition - and the PBS’s reference pricing system. The PBS groups similar drugs into “price disclosure groups.” The government only pays up to the lowest-priced option in that group. So if you’re prescribed a brand-name drug, but a cheaper generic exists, the pharmacist will give you the generic unless you specifically ask for the brand. And even then, you pay the difference out of pocket. This system pushed Australia’s generic use rate above the OECD average. But it’s not perfect. Some therapeutic areas - like biologics for rheumatoid arthritis or multiple sclerosis - still have low generic uptake. Why? Because these drugs are complex. You can’t just copy them like a simple pill. And the PBS hasn’t fully caught up with how to evaluate or reimburse them.Who Pays What - And Why It Matters
As of July 2024, the co-payment for a PBS medicine was $31.60 for general patients and $7.70 for concession card holders. That sounds low - until you realize most people with chronic conditions take five or six meds a month. A self-funded retiree on five PBS drugs? That’s $158 a month just in co-payments. No wonder 12.3% of general patients skip doses or don’t fill prescriptions because of cost, according to the 2024 National Health Survey. That’s over 1.8 million Australians choosing between medicine and groceries. The safety net helps. Once you hit $1,571.70 in out-of-pocket costs for PBS medicines in a year, your co-payment drops to $7.70 - no matter what. But you have to track it. Most people don’t. And if you’re not on a concession card, you’re stuck with the higher rate. The good news? The National Health Amendment (Cheaper Medicines) Bill 2025 passed in May 2025. Starting January 1, 2026, the general patient co-payment drops to $25. That’s a $6.60 cut - and it’ll save Australians nearly $800 million over four years. But it also means the government will spend an extra $689 million. Someone’s paying.
Why New Drugs Take So Long to Arrive
If you’re diagnosed with a rare cancer and a new drug is approved in the U.S. or Europe, you might expect it to be available in Australia within months. You’d be wrong. The median time from global launch to PBS listing? 587 days. That’s nearly two years. In Germany? 320 days. In Canada? 410. Why the delay? Three big reasons. First, the PBAC review process is thorough - but slow. They need clinical trial data, cost-effectiveness models, budget impact forecasts. Second, drug companies often delay applying for PBS listing because they want to maximize profits in the private market first. Third, the PBS doesn’t fast-track drugs unless they’re for life-threatening conditions with no alternatives. That’s why patients with rare diseases often pay $1,850 out-of-pocket for 14 months while waiting for approval. The Highly Specialised Drugs Program (HSDP) was meant to fix this, but its eight strict criteria - including requirements around life expectancy and disease severity - still block access for many. A November 2025 reform will ease two of those criteria. It’s a start.The Real Cost of Bureaucracy
Behind every PBS script is paperwork. A lot of it. About 28% of PBS-listed medicines require “authority required” status. That means the doctor must submit a form - online or paper - explaining why this patient needs this specific drug. Pharmacists process 17.3 PBS transactions a day on average. Nearly 70% say authority scripts slow them down. One pharmacist in Adelaide told me: “I’ve had patients cry because they had to wait three days for approval. They’re running out of pills. I can’t just give them more.” The online system processes 2.1 million authority requests a month. Electronic approvals take 1.8 business days. Paper? 7.3 days. And if the form is wrong? Back to square one. Doctors aren’t immune. The Australian Medical Association says new prescribers need 40 hours of training just to understand PBS rules. That’s not in med school. That’s on the job. And it’s exhausting.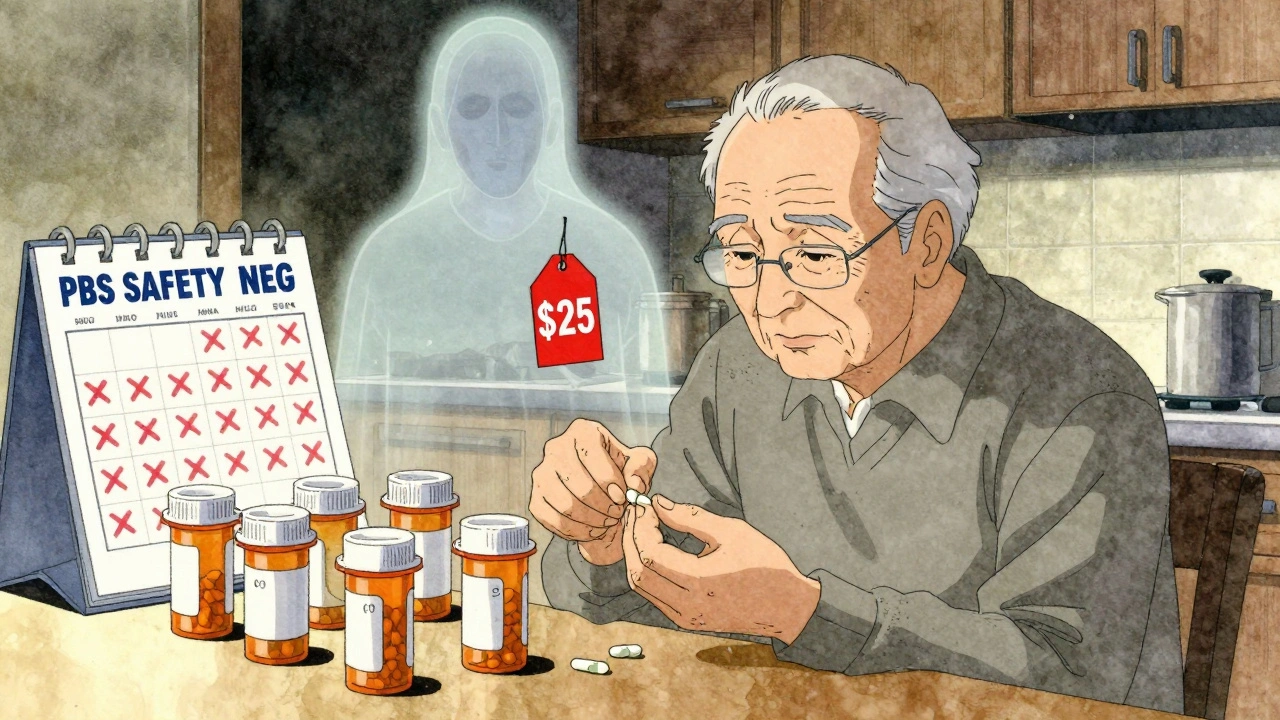
Who Wins? Who Loses?
The PBS is a success story - but not for everyone. Winners:- Concession card holders - they pay $7.70 and get 60-day scripts.
- People with chronic diseases - 98% of hypertension meds and 95% of diabetes meds are generics on the PBS.
- Pharmacists - they get paid for every script, and generics are easier to dispense.
- Taxpayers - the PBS saves households an estimated $13 billion a year in out-of-pocket costs.
- General patients without concession status - $25 or $31.60 per script adds up fast.
- People with rare diseases - the HSDP still leaves too many behind.
- Doctors - burdened by administrative work.
- Drug companies - they can’t charge what they want. Profit margins are squeezed.
What’s Next?
The PBS is changing. Fast. In 2025-26, the government added $1.2 billion to list new drugs like Talazoparib for prostate cancer and Relugolix for endometriosis. That’ll help 150,000 more Australians. But it also means spending will keep rising - projected to hit $18.7 billion by 2029-30. The Department of Health is rolling out AI tools to spot inappropriate prescriptions. Right now, $1.2 billion a year is spent on drugs that may not be needed. That’s waste. The goal? Cut it in half. Real-time prescription monitoring is coming. Pharmacists will see if a patient is getting the same drug from multiple doctors. That’s to stop misuse - but also to help patients who are overprescribed. The big question? Can Australia keep this system going? Dr. John Skerritt, former Deputy Secretary of Health, warned that PBS spending could hit 2.6% of GDP by 2045. That’s triple the 0.7% it was in 2005. With an aging population and more expensive drugs, the math doesn’t add up unless prices are controlled harder - and faster.What You Can Do
If you’re on the PBS:- Check if your meds are on the PBS list - go to pbs.gov.au (updated monthly).
- Use the PBS App. It tracks your co-payments and tells you when you’re close to the safety net.
- Ask your pharmacist: “Is there a generic version?” If yes, you’ll save money.
- If you’re on five or more PBS scripts, apply for a concession card if you qualify.
- Call 1800 020 299 if you’re confused. They handle 1.7 million calls a year. Wait time? Under 4 minutes.
How much do Australians pay for PBS medicines in 2025?
As of July 2024, general patients pay $31.60 per PBS script, and concession card holders pay $7.70. These amounts are indexed to inflation each year. However, starting January 1, 2026, the general co-payment will drop to $25.00 under the National Health Amendment (Cheaper Medicines) Bill 2025. Concession co-payments remain unchanged.
What is the PBS safety net?
The PBS safety net is a cap on out-of-pocket costs for prescription medicines. In 2025, once a general patient spends $1,571.70 on PBS scripts in a calendar year, they qualify for reduced co-payments of $7.70 for the rest of the year. Concession card holders automatically get the lower rate regardless of spending. You don’t need to apply - Services Australia tracks your spending automatically.
Why are some medicines not on the PBS?
A medicine must pass strict criteria to be listed: proven clinical effectiveness, cost-effectiveness (typically under AU$50,000 per quality-adjusted life year), and budget impact. Many new drugs, especially for rare diseases or with high price tags, don’t meet these thresholds. Some are also not submitted for listing by manufacturers because they want to profit in the private market first.
Are generic drugs as good as brand-name drugs?
Yes. Generic drugs contain the same active ingredients, dosage, and strength as their brand-name counterparts. They’re required to meet the same quality standards set by the Therapeutic Goods Administration (TGA). The only differences are in inactive ingredients (like fillers) and packaging. For 95% of medications, generics are clinically identical.
How does the PBS compare to other countries?
Australia’s PBS is more restrictive than the U.S. but more flexible than the UK’s NICE system. While the UK uses a strict £20,000-£30,000 per QALY threshold, Australia’s unofficial $50,000 threshold allows more high-cost drugs to be approved, especially for rare diseases. Australia’s drug prices are 30-40% lower than the U.S. but 15-20% higher than the UK’s NHS. The PBS’s reference pricing system drives higher generic use than most OECD countries.
Can I get PBS medicines if I’m not an Australian citizen?
Yes, if you’re from one of the 11 countries with a Reciprocal Health Care Agreement with Australia: New Zealand, United Kingdom, Ireland, Sweden, Netherlands, Finland, Italy, Malta, Norway, Slovenia, and Belgium. You must have a valid Medicare card from your home country and be visiting Australia temporarily. Tourists and students from other countries are not covered.
Why do some PBS scripts take days to approve?
Scripts marked as “authority required” need prior approval from Medicare Australia. This applies to high-cost drugs, restricted-use medications, or those with safety concerns. Electronic applications take 1.8 business days; paper applications take over 7 days. Delays happen if the form is incomplete or if additional clinical information is requested.
How often does the PBS add new medicines?
The PBS adds new medicines regularly - usually monthly. In 2025, 150,000 Australians gained access to new drugs like Talazoparib and Relugolix. The PBAC meets every two months to review submissions. On average, 30-50 new drugs are listed each year, with about 10-15 being generics.





Angela R. Cartes
December 9, 2025 AT 07:54