Clozapine Dose Adjustment Calculator
Dose Adjustment Calculator
This tool helps estimate appropriate clozapine dose adjustments based on smoking status. Always consult with your healthcare provider before making any medication changes.
If you’re taking clozapine and you smoke, your medication might not be working like it should. Not because it’s broken. Not because you’re doing anything wrong. But because tobacco smoke is quietly changing how your body processes the drug. This isn’t a myth. It’s not a warning on a pamphlet you ignored. It’s a well-documented, clinically significant interaction that can mean the difference between symptom control and hospitalization.
Why Clozapine Is So Sensitive to Smoking
Clozapine is one of the most effective antipsychotics for treatment-resistant schizophrenia. But it’s also one of the trickiest to manage. About 60 to 70% of clozapine is broken down by a single liver enzyme: CYP1A2. That’s unusually high. Most drugs are handled by multiple enzymes, so if one slows down, others can pick up the slack. Clozapine doesn’t have that safety net. If CYP1A2 speeds up, clozapine levels crash. Tobacco smoke contains chemicals like polycyclic aromatic hydrocarbons. These bind to a receptor in your liver called AhR. That triggers your body to make more CYP1A2 enzyme. More enzyme means faster breakdown. Studies show that smokers on clozapine have, on average, 30% lower blood levels than non-smokers. Some people see drops as high as 50%. That’s not a small fluctuation. It’s enough to push levels below the therapeutic range of 350-500 ng/mL.What Happens When You Start or Quit Smoking
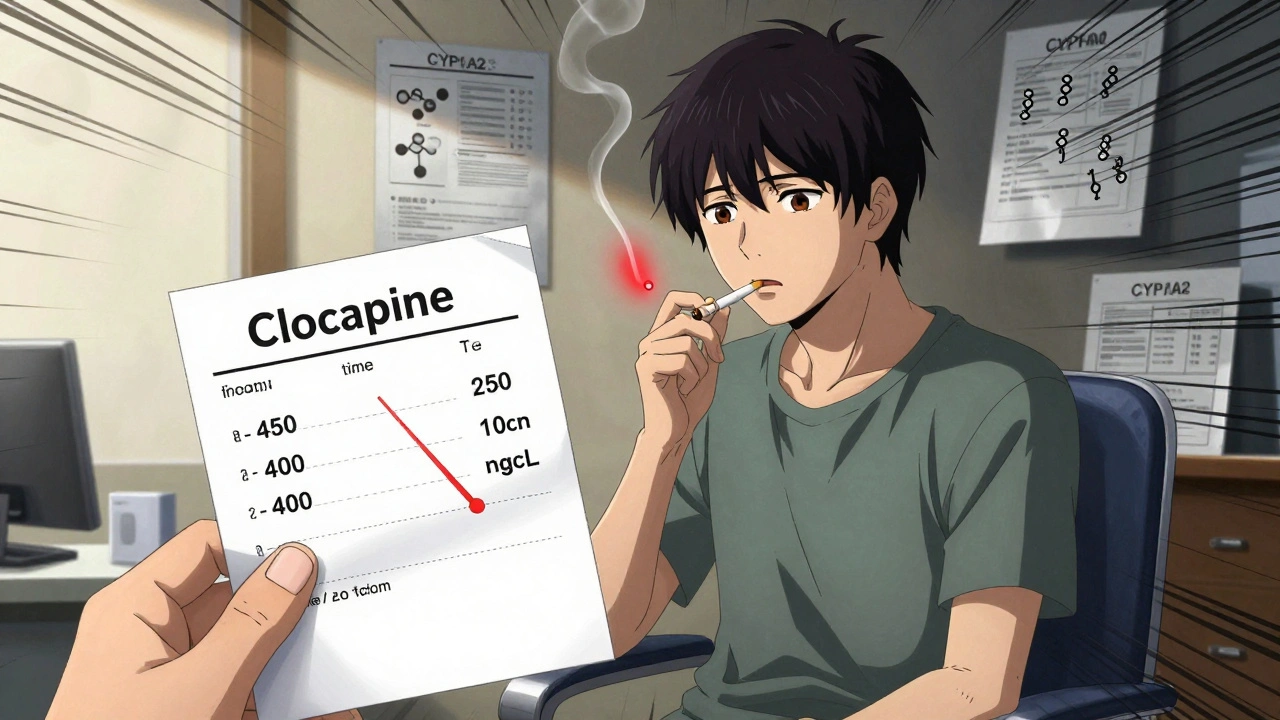
This isn’t a slow, gradual change. The enzyme induction kicks in within 48 to 72 hours of starting to smoke regularly. If you pick up smoking after being a non-smoker, your clozapine levels can drop fast. One patient reported his levels falling from 400 ng/mL to 150 ng/mL in just two weeks. His symptoms returned - hallucinations, disorganized thinking - and he ended up back in the hospital. The reverse is just as dangerous. When someone quits smoking, CYP1A2 activity doesn’t drop overnight. It takes 1 to 2 weeks to return to baseline. If their clozapine dose hasn’t been lowered, levels start climbing. That’s when toxicity hits: extreme drowsiness, rapid heartbeat, seizures, or even life-threatening conditions like myocarditis or agranulocytosis. A 45-year-old woman in a 2022 case study developed clozapine toxicity at 850 ng/mL - more than double the upper limit - after quitting smoking while staying on her 400 mg daily dose. She needed a 37% dose reduction to recover.It’s Not Just Cigarettes
Many assume vaping or nicotine patches are safe alternatives. They’re not. Research from the University of Toronto in June 2024 showed that e-cigarettes induce CYP1A2 too - just slightly less than traditional cigarettes. If you switch from smoking to vaping and don’t adjust your dose, you’re still at risk of subtherapeutic levels. Nicotine gum or patches don’t trigger this effect, since they don’t contain the polycyclic aromatic hydrocarbons that induce the enzyme. But if you’re using e-cigarettes, treat them like tobacco.How Doctors Manage This
The only reliable way to handle this is through therapeutic drug monitoring. That means regular blood tests to measure clozapine levels. The American Psychiatric Association recommends checking levels 4 to 7 days after any dose change. If you start smoking, expect your dose to go up by 40 to 60%. A patient on 300 mg might need 450 to 500 mg. If you quit, reduce your dose by 30 to 50%. A 500 mg dose might need to drop to 250-350 mg. Most psychiatrists who regularly prescribe clozapine check smoking status at every visit. A 2023 survey of clinicians found 68% do this routinely, and 82% adjust doses based on smoking changes. Electronic health records now include alerts for this interaction. One 2023 study in JAMA Internal Medicine showed these alerts cut adverse events by 37%.
Genetics Make It Even More Complex
Not everyone responds the same way. Some people have a genetic variant called CYP1A2 *1F/*1F. On its own, this doesn’t change baseline enzyme activity. But when exposed to tobacco smoke, their CYP1A2 becomes hyper-responsive. Their clozapine levels drop more than average - sometimes 50% or more. This isn’t rare. About 1 in 3 people of European descent carry this variant. Without genetic testing, you might assume a patient is just a heavy smoker. But it could be genetics amplifying the effect.What About Other Antipsychotics?
Olanzapine is also metabolized by CYP1A2, so smoking affects it too - but less dramatically. Clozapine’s therapeutic window is narrower, and CYP1A2 handles a larger share of its metabolism. Risperidone? Mostly broken down by CYP2D6. Smoking doesn’t touch it. Quetiapine? Primarily handled by CYP3A4. Aripiprazole? CYP2D6 and CYP3A4. These might be safer choices if you’re trying to quit smoking and don’t want to risk dose swings. But here’s the catch: clozapine is still the most effective drug for treatment-resistant schizophrenia. If other medications failed, switching isn’t always an option. That’s why managing the smoking interaction is so critical.Real-World Stories
A Reddit user in March 2023 wrote: “I tried to quit smoking three times. Each time, I got so sedated I couldn’t stand up. My doctor didn’t lower my dose fast enough. I ended up in the ER.” Another shared: “Once my doctor figured out the smoking connection and bumped my dose up, my symptoms stabilized for the first time in five years.” These aren’t outliers. They’re common. A 2021 Health Affairs study found that unmanaged clozapine-smoking interactions led to 22% higher hospitalization rates. Each avoidable admission costs about $14,500.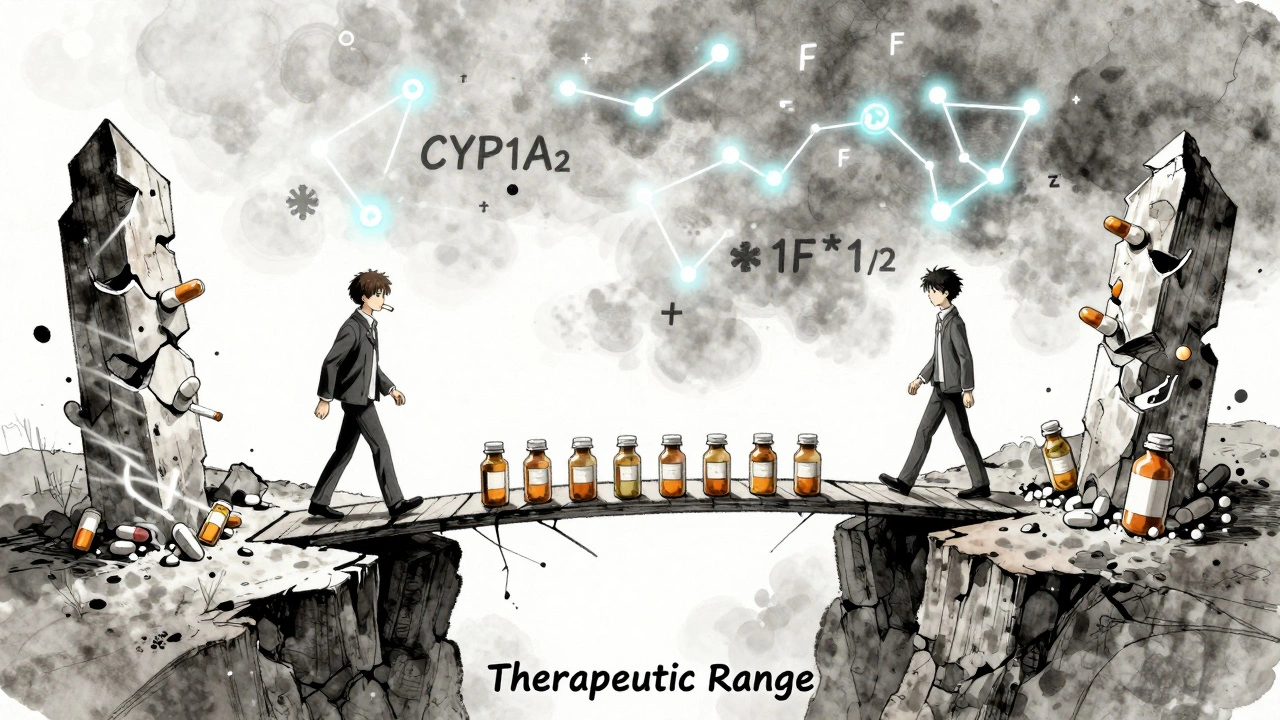
What You Can Do
If you’re on clozapine:- Be honest with your doctor about smoking, vaping, or quitting.
- Ask for a baseline clozapine level if you haven’t had one.
- Request follow-up levels 1 week after any change in smoking habits.
- Don’t assume vaping is safe - it still affects CYP1A2.
- If you’re trying to quit, talk to your doctor about adjusting your dose before you stop.
- Ask if pharmacogenetic testing for CYP1A2 is available. It’s not standard everywhere, but it’s growing.
The Bigger Picture
About 60 to 70% of clozapine patients smoke - compared to just 14% of the general U.S. population. That’s not a coincidence. People with serious mental illness are more likely to smoke, often as a form of self-medication. But this interaction turns a coping mechanism into a medical risk. Researchers are working on solutions. A 2024 clinical trial is testing a sustained-release clozapine formulation designed to smooth out the peaks and valleys caused by CYP1A2 induction. Early results show 40% less variability in blood levels among smokers. The FDA now treats this interaction as a model case for how environment, genes, and drugs interact. That means future guidelines will likely push for more routine testing and personalized dosing. But right now, the tools we have are simple: blood tests, dose adjustments, and honesty. No fancy tech. No magic pills. Just careful monitoring and communication.Frequently Asked Questions
Does nicotine alone affect clozapine levels?
No. Nicotine itself doesn’t induce CYP1A2. It’s the other chemicals in tobacco smoke - like polycyclic aromatic hydrocarbons - that trigger the enzyme increase. That’s why nicotine patches or gum don’t interfere with clozapine, but cigarettes and e-cigarettes do.
How long after quitting smoking should I wait before lowering my clozapine dose?
Don’t wait. Start reducing your dose as soon as you quit, but do it gradually. CYP1A2 enzyme levels take 1 to 2 weeks to return to normal. Your doctor should lower your dose by 30-50% right away and recheck your blood levels after 7-10 days. Waiting too long risks toxic buildup.
Can I just stop smoking to avoid the problem?
Quitting smoking is a good goal - but not without planning. Stopping suddenly while on a high clozapine dose can lead to dangerous toxicity. Talk to your psychiatrist before quitting. They may lower your dose in advance or use a slower taper. Support programs for smoking cessation in psychiatric patients are available and more effective when coordinated with your medication team.
Are there any foods or supplements that affect CYP1A2?
Yes. Grapefruit juice inhibits CYP3A4, but not CYP1A2. Cruciferous vegetables like broccoli and Brussels sprouts can mildly induce CYP1A2, but not nearly as much as smoking. Caffeine is metabolized by CYP1A2, so if you’re a heavy coffee drinker, your doctor might use caffeine levels as a rough indicator of enzyme activity - but blood tests for clozapine are still the gold standard.
What if my doctor doesn’t know about this interaction?
Bring up the research. Cite the FDA’s prescribing information, which specifically warns about tobacco smoke reducing clozapine levels. Mention that the European Medicines Agency classifies this as a "clinically significant" interaction requiring dose adjustment. If your doctor isn’t familiar, ask for a referral to a psychiatrist who specializes in psychopharmacology or therapeutic drug monitoring.




Elizabeth Crutchfield
December 5, 2025 AT 18:00