Ever wonder why a pill you swallow turns into relief - or why the same drug works for your friend but gives you a rash? It’s not magic. It’s pharmacology. And understanding how medications work isn’t just for doctors or pharmacists - it’s key to using them safely, avoiding dangerous interactions, and knowing when something’s not right.
What Pharmacology Really Means
Pharmacology is the science of how chemicals - whether made in a lab or pulled from a plant - interact with your body. It’s not just about what drugs do. It’s about how they get there, how they change your cells, and why sometimes they cause side effects instead of healing. This field started in the 1800s with Oswald Schmiedeberg, who set up the first lab in Strasbourg to test drugs on animals. Today, it’s the backbone of nearly every medicine you’ve ever taken. In fact, 92% of drugs approved by the FDA between 2010 and 2020 were developed using pharmacological research. That means every antibiotic, painkiller, or antidepressant you use was designed based on how molecules bind, block, or trigger reactions inside your body. It’s not guesswork. It’s precision science. And that precision is what keeps you safe - or puts you at risk if it’s ignored.The Two Sides of the Coin: Pharmacokinetics and Pharmacodynamics
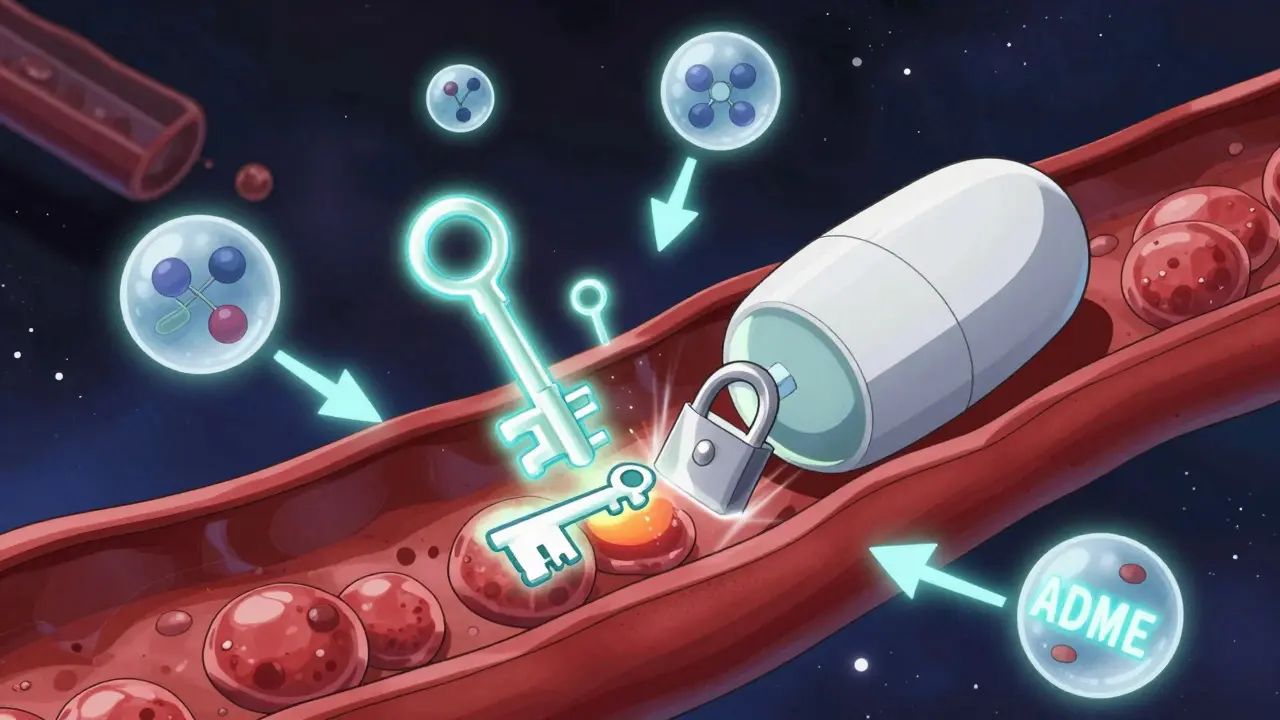
Pharmacology breaks down into two big parts: what your body does to the drug, and what the drug does to your body. The first is pharmacokinetics - think of it as the drug’s journey through you. It follows four steps, remembered by the acronym ADME:- Absorption: How the drug gets into your bloodstream. A pill swallowed in the stomach might take 30 minutes to an hour to start working. An injection? Almost immediate.
- Distribution: Once in the blood, the drug travels. Some drugs cross the blood-brain barrier to affect your mind. Others stay in your muscles or liver.
- Metabolism: Your liver breaks the drug down. Enzymes like CYP450 are the main workers here. But not everyone has the same enzymes. About 17% of people have genetic differences that make them slow or fast metabolizers - which can turn a normal dose into an overdose or useless.
- Excretion: What’s left gets flushed out - mostly through kidneys or bile. If you have kidney disease, drugs can build up. That’s why doctors adjust doses for older adults or people with organ issues.
How Drugs Actually Talk to Your Body
Your body is full of proteins that do jobs: some carry oxygen, some build bones, and others act like switches. Drugs work by interacting with these switches - mostly receptors, enzymes, and transporters. About 60% of drugs target receptors. These are like locks on the surface of your cells. The drug is the key.- Agonists turn the switch on. For example, morphine binds to opioid receptors and tells your brain to stop feeling pain.
- Antagonists block the switch. Beta-blockers like metoprolol sit on heart receptors and prevent adrenaline from speeding up your pulse - that’s how they lower blood pressure.
- Partial agonists turn the switch partway. Buprenorphine, used for opioid addiction, gives just enough effect to reduce cravings without causing a high.
- Inverse agonists do the opposite of what the natural signal does. Some anti-anxiety drugs work this way.

Why Two People React So Differently
You and your neighbor take the same antidepressant. You feel better. They feel sick. Why? It’s not luck. It’s pharmacogenetics. Your genes determine how fast your liver breaks down drugs. If you’re a slow metabolizer of warfarin - a blood thinner - even a tiny dose can cause dangerous bleeding. Fast metabolizers might need twice the dose to get the same effect. That’s why genetic testing is becoming part of prescribing for certain drugs. Age matters too. Older adults often have weaker kidneys and livers. A dose that’s fine for a 30-year-old can build up in someone 70 and cause confusion or falls. And then there’s polypharmacy. One in three adults over 65 takes five or more medications. Each one adds risk. A common painkiller like ibuprofen can interfere with blood pressure meds. An antibiotic can make birth control fail. These aren’t rare mistakes. They’re predictable - if you know how the drugs work.What Happens When Pharmacology Is Ignored
In 2023, a study of 12,500 patients found that when doctors adjusted drug doses based on kidney or liver function, adverse drug events dropped by 27%. That’s 1 in 4 fewer hospital visits - all because someone checked the basics. But when pharmacology is misunderstood, the results are deadly. One Reddit user, a nursing student, shared how a patient on an MAOI (an old antidepressant) was given an SSRI - a common new antidepressant. Both increase serotonin. Together, they caused serotonin syndrome: high fever, seizures, muscle rigidity. The patient nearly died. The staff didn’t realize the combination was dangerous because they didn’t understand the pharmacodynamics. Another case: a man on statins for cholesterol took a common antibiotic called clarithromycin. The antibiotic blocked the enzyme that breaks down statins. His blood levels spiked. He developed rhabdomyolysis - his muscles started breaking down. His kidneys failed. He survived, but only because his doctor caught it early. These aren’t horror stories. They’re textbook pharmacology failures.
What’s New in How Drugs Work
The field isn’t standing still. In 2024, DeepMind’s AlphaFold 3 could predict how drugs bind to proteins with 89% accuracy - up from 67% just two years ago. That means faster drug discovery, fewer dead ends, and better-targeted treatments. The FDA has approved 12 new biomarkers to measure how drugs behave in real time - especially for kidney patients. No more guessing. Now they can see exactly how a drug is cleared. And biologics - drugs made from living cells - are changing everything. These aren’t pills. They’re injections or infusions that block specific immune signals, like TNF-alpha or interleukins. They’re used for rheumatoid arthritis, Crohn’s, psoriasis. They account for 35% of all new drugs approved since 2015. They’re expensive. But they work where pills don’t.What You Can Do
You don’t need a medical degree to use meds safely. But you do need to ask the right questions:- What is this drug supposed to do? Is it blocking a receptor? Stopping an enzyme? Pulling water into your gut?
- What should I watch for? Side effects aren’t random. They’re often the drug working where it shouldn’t - like aspirin irritating your stomach because it blocks protective enzymes there.
- What else am I taking? Write down every pill, supplement, and herb. Even St. John’s Wort can interfere with antidepressants.
- Do I have kidney or liver issues? If yes, ask if your dose needs to change.
The Bottom Line
Medications aren’t just pills. They’re complex tools. Understanding how they work - not just that they work - gives you power. Power to avoid harm. Power to speak up. Power to make smarter choices. The science is advanced. But the basics haven’t changed. Your body has receptors. Your liver has enzymes. Your kidneys filter. If you know how drugs interact with those, you’re not just a patient. You’re an informed partner in your care.And in a world where drug interactions kill more people than car accidents every year - that knowledge isn’t optional. It’s essential.





Janette Martens
December 29, 2025 AT 07:04