When your knees ache every time you stand up, or your hips stiffen after sitting too long, it’s easy to think surgery or pills are the only answers. But the truth is, physical therapy is often the most effective, longest-lasting solution for joint disorders - and it’s backed by more than a decade of hard data. It’s not just about stretching or doing a few reps. It’s a science-backed, personalized plan that rebuilds movement, reduces pain, and keeps you active - without drugs or knives.
Why Movement Is Medicine
For years, joint pain was treated as a symptom to suppress. Painkillers, injections, and eventually surgery were the go-to fixes. But research has flipped that script. The American College of Rheumatology’s 2021 guidelines made it clear: movement isn’t just helpful - it’s disease-modifying. For people with rheumatoid arthritis, sticking to a prescribed exercise routine slows joint damage by 23%. That’s not a side effect. That’s treatment.
Same goes for osteoarthritis. A 2023 study in Arthritis & Rheumatology found that physical therapy delivered the same functional improvement as a total hip replacement for mild-to-moderate cases. The only difference? You skip the hospital stay, the recovery time, and the risk of infection. And you save thousands. Medicare data shows patients who do physical therapy before knee replacement have 22% lower total care costs. This isn’t a last resort. It’s the first line of defense.
Range of Motion: The Foundation
Joint stiffness isn’t just annoying - it’s a trap. When you stop moving, your muscles tighten, your cartilage loses lubrication, and your joint capsule shrinks. That’s when pain gets worse, and mobility drops fast.
Range of motion (ROM) exercises aren’t about touching your toes. They’re about restoring the natural glide of your joint. For knee osteoarthritis, the gold standard is terminal knee extension: slowly straightening the knee from a 20-degree bend to full extension. Do 3 sets of 10 to 15 reps, five days a week. Use just enough resistance - like a 2.5kg ankle weight - to feel the burn, but not the pain. Keep pain under 3 out of 10 on the scale. If it’s higher, you’re pushing too hard.
For hips, slow hip circles and seated knee-to-chest stretches help restore the joint’s natural rotation. These aren’t flashy moves. But they’re the ones that matter. The 2025 JOSPT Hip Pain guideline recommends doing them daily, with attention to control, not speed. The goal? Regain the ability to put on socks, climb stairs, or sit in a car without wincing.
Strengthening: Build the Support System
Your muscles are your body’s natural braces. When they’re weak, your joints take the stress. Strengthening isn’t about lifting heavy. It’s about loading the joint correctly so your body learns to protect itself.
For hip OA, hip abductor strengthening is key. That’s the muscle on the side of your thigh that keeps your pelvis level when you walk. The protocol? 3 sets of 15 reps with 2.5 to 5kg resistance, three times a week. Use a resistance band or a machine. Don’t rush. Focus on the squeeze at the top of each rep.
For knees, quad sets and straight leg raises are simple but powerful. Lie on your back, tighten your thigh muscle, and lift your leg six inches off the ground. Hold for 5 seconds. Lower slow. Do 15 reps. Three times a day. That’s it. No gym needed.
The American College of Rheumatology recommends resistance training at 40-60% of your one-rep max for major muscle groups, twice a week. That’s not bodybuilding. That’s joint preservation.

What Works - And What Doesn’t
Not all physical therapy is created equal. A 2022 meta-analysis in the Annals of Family Medicine found that for sacroiliac joint dysfunction, combining exercises with manual manipulation led to 68% pain reduction after a year. NSAIDs? Only 32%. The number needed to treat - meaning how many people you need to treat to get one person significantly better - was 2.8. That’s better than most medications.
But there’s a catch. Generic exercises? They fail. Dr. Thomas Schnitzer, former president of the Osteoarthritis Research Society International, says generic programs only work for 12-15% of people. Personalized plans? 65-70% success rate. That’s why a good physical therapist doesn’t hand you a handout. They test your movement, measure your strength, and adjust every week.
And here’s the hard truth: if your joint space is more than 50% narrowed on an X-ray, exercise alone won’t fix it. That’s not failure. That’s reality. But even then, therapy can delay surgery by years - and make recovery smoother when you do go under the knife.
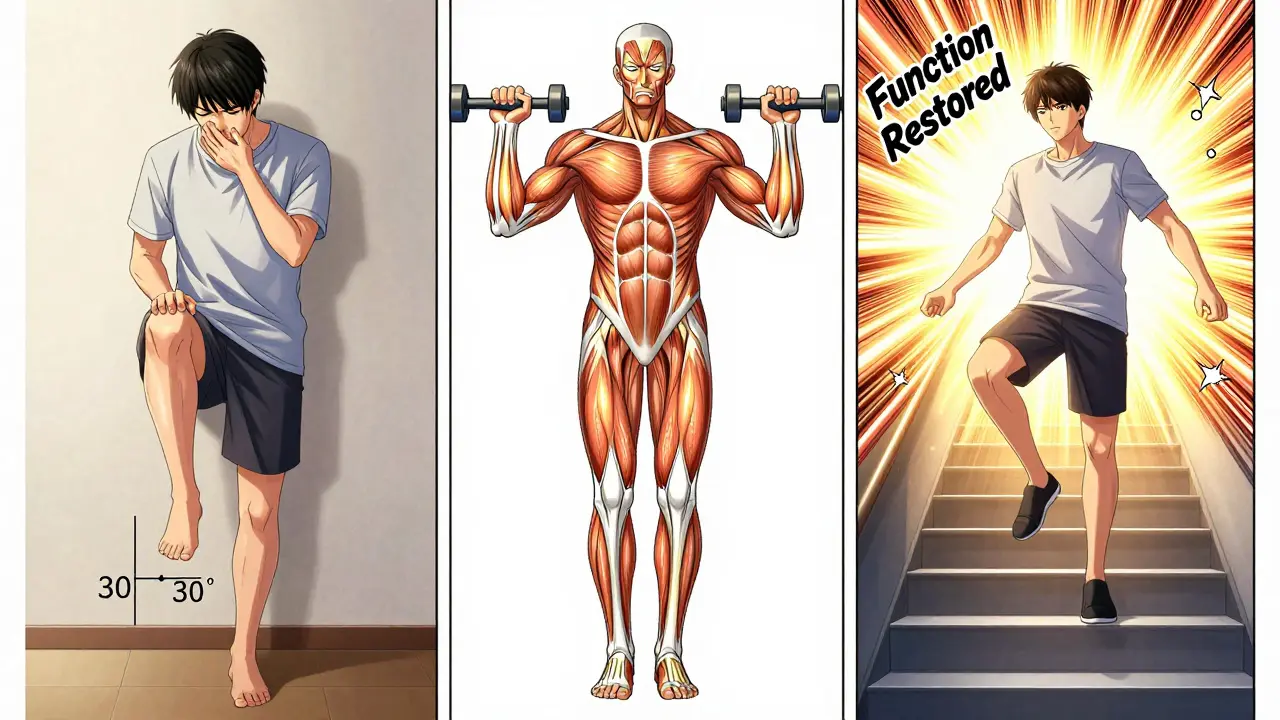
The Phases: From Pain to Power
Physical therapy doesn’t happen in one step. It follows a clear path:
- Acute Phase (0-2 weeks): Focus on pain control and gentle motion. For a stiff knee, that might mean 0-30 degrees of extension. No resistance. Just movement.
- Subacute Phase (2-6 weeks): Introduce isometric holds. Tighten muscles without moving the joint. Think: quad sets, glute squeezes. Build endurance without strain.
- Functional Phase (6+ weeks): Now you add dynamic strength. Squats, step-ups, resistance bands. Progress to 60-80% of your max effort. This is where you regain real-world function - walking, climbing, standing up from a chair.
Medicare data shows most people hit their goals by session 12 - if they stick to the plan. The key? Consistency. You need to complete at least 70% of your prescribed exercises. Miss too many, and the benefit fades.
Technology Is Changing the Game
Therapy isn’t just in the clinic anymore. New tools are making it smarter.
The 2025 JOSPT Hip Osteoarthritis guideline introduced machine learning algorithms that predict how well you’ll respond to specific exercises - based on your HOOS score, BMI, and X-ray results. It’s 83% accurate. That means your therapist can skip the guesswork and start with what works for you.
And with new Medicare billing codes effective January 2025, you can now get reimbursed for remote therapy using wearable sensors. These devices track your movement accuracy in real time. If your squat angle is off by 5 degrees, your app alerts you. No more hoping you’re doing it right.
Even more promising? A 2024 University of Pittsburgh study found that combining physical therapy with neuromuscular electrical stimulation (NMES) boosted strength gains by 41% over exercise alone. It’s not magic. It’s science. NMES gently fires your muscles while you rest, helping rebuild strength faster.
Barriers - And How to Overcome Them
Despite the evidence, many people quit. Why? Three big reasons:
- Insurance limits. 58% of negative reviews on Yelp mention session caps. Some plans only cover 10 visits. That’s not enough. Advocate. Ask your therapist to appeal. Many insurers will extend coverage if you show progress.
- Transportation. Rural patients are 2.4 times more likely to drop out. If you can’t get to a clinic, ask about telehealth. Remote monitoring with sensors works.
- Initial pain. 41% of Reddit users report pain getting worse in the first two weeks. That’s normal. Your muscles are waking up. But if pain spikes above 5/10 or lasts more than 24 hours, tell your therapist. Adjustments are easy.
And don’t wait. The Arthritis Foundation says 78% of rheumatologists now refer patients to physical therapy within six months of diagnosis. That’s up from 42% in 2015. The sooner you start, the more you save - in pain, money, and mobility.
What Success Looks Like
Real improvement isn’t about lifting more weight. It’s about doing what you couldn’t before:
- Getting out of bed without grabbing the railing
- Climbing stairs without stopping
- Standing for 10 minutes while cooking
- Walking the dog without limping
On Healthgrades, physical therapy for joint disorders has a 4.2/5 rating from over 14,000 reviews. 68% of users say they saw significant improvement in daily function within 8 weeks. That’s not hype. That’s data.
And the future? It’s bright. Starting in 2026, Medicare will cover maintenance therapy for chronic joint conditions. That means ongoing sessions - not just a short burst. CMS is also mandating 8 sessions of therapy before approving knee replacement. That’s policy catching up to science.
Physical therapy for joint disorders isn’t about fixing broken joints. It’s about rebuilding the body’s natural ability to move. It’s not glamorous. But it works. And it’s the most powerful tool you have - before you ever need a needle, a shot, or a scalpel.
How long does physical therapy take for joint pain?
Most people see noticeable improvement within 4 to 8 weeks. Medicare data shows 87% of patients with knee osteoarthritis reach their functional goals by session 12. A full course typically lasts 14 to 16 sessions, but this varies by condition. Hip OA may need 12-20 sessions; rheumatoid arthritis often requires ongoing maintenance.
Can physical therapy replace surgery for joint disorders?
For mild-to-moderate osteoarthritis, yes - in terms of function. A 2023 study found physical therapy matched the outcomes of total hip replacement at 12 months. It doesn’t reverse joint damage, but it can delay surgery by an average of 2.7 years. For advanced cases with severe cartilage loss, surgery may still be necessary, but pre-surgery therapy improves outcomes and cuts recovery time.
Is it normal to feel more pain at first during physical therapy?
Yes, for some. About 41% of patients report increased pain in the first 1-2 weeks as muscles reawaken and joints adjust. Pain should stay under 5/10 and fade within 24 hours. If it lasts longer, gets worse, or causes swelling, tell your therapist. It may mean the intensity is too high, or the technique needs adjustment. Never push through sharp or joint-specific pain.
What if my insurance won’t cover enough physical therapy sessions?
Many insurers cap visits at 10-20, which is often insufficient. Ask your therapist to submit a letter of medical necessity - citing specific functional goals and outcome measures like HOOS or Six-Minute Walk Test improvements. Many insurers approve extensions if you show measurable progress. You can also explore community clinics, university training programs, or telehealth options that may be more affordable.
Can I do physical therapy at home?
Yes - but only after a proper assessment. Home programs work best when they’re personalized and monitored. Use validated apps with wearable sensors (like those covered by Medicare since 2025) to ensure correct form. Generic YouTube videos rarely work - they don’t account for your specific joint alignment or muscle weakness. A single session with a licensed therapist to set up your home routine is worth it.






