Why Your Skin Is Reacting to the Cream You’re Using
You put on the cream your doctor prescribed for your eczema. A few days later, your skin gets redder, itchier, and starts flaking. You think it’s getting worse-so you apply more. But it doesn’t help. In fact, it gets worse. That’s not your eczema flaring up. That’s your skin having an allergic reaction to the medication itself.
This isn’t rare. Around 1 in 6 people who get patch tested for stubborn skin rashes turn out to be allergic to something in their topical medicine. And the worst part? Most doctors don’t suspect it. They assume the treatment can’t be the problem. But it can-and often is.
Topical medication allergies cause a type of skin reaction called allergic contact dermatitis. It’s not an immediate burn or rash. It shows up slowly-usually 24 to 72 hours after contact. The skin becomes red, swollen, itchy, and sometimes blistered. It looks like a bad case of eczema, but it’s not. It’s your immune system reacting to a drug you thought was helping you.
What Causes Topical Medication Allergies?
It’s not just the active ingredient. The problem can come from the medicine itself-or from the preservatives, fragrances, or even the base cream it’s mixed into. But the biggest culprits are well-known.
- Antibiotics: Neomycin is the most common. Found in over-the-counter ointments like Neosporin, it triggers reactions in nearly 10% of patch-tested patients. Bacitracin and gentamicin are close behind.
- Corticosteroids: Ironically, these are the go-to treatment for skin inflammation. But about 1 in 50 people who use them develop an allergy to them. Hydrocortisone, triamcinolone, and clobetasol are frequent offenders.
- Local anesthetics: Benzocaine, used in numbing creams for sunburns or hemorrhoids, causes reactions in over 2% of tested patients.
- NSAIDs: Ketoprofen, found in some topical pain gels, is a hidden trigger. People don’t realize it’s in their back rub or knee cream.
Here’s the twist: you can be allergic to one steroid but not another. Steroids are grouped into six categories based on their chemical structure. If you’re allergic to hydrocortisone (Group A), you can often safely use triamcinolone (Group B) or methylprednisolone (Group D). Knowing this saves people from avoiding all steroids unnecessarily.
How Is It Diagnosed?
Most doctors won’t test for this unless you push for it. But if your rash keeps coming back-or gets worse after using a treatment-it’s time to ask for a patch test.
Here’s how it works: small patches containing common allergens, including 20-30 topical medications, are taped to your back. You leave them on for 48 hours. Then they’re removed, and your skin is checked. You come back at 72 hours and sometimes even 96 hours later because reactions can be delayed.
It’s not painful. It’s not dangerous. But it’s the only way to know for sure what’s causing your rash. And it works-about 70% of the time. In one study, 15-20% of people who thought they had a medication allergy actually had irritant dermatitis, not an allergy. That’s why testing matters. You don’t want to avoid a drug you can safely use… or keep using one you’re allergic to.
And don’t forget: your shampoo, lotion, or hand sanitizer might be the problem too. Many people don’t realize that a fragrance in their moisturizer or a preservative in their face wash can be the trigger. That’s why experts say: bring everything you put on your skin to your appointment.

Treatment: Stop the Allergen, Then Soothe the Skin
The most important step? Stop using the allergen. No exceptions. Even if it’s a prescription. Even if your doctor says it’s the best option. If your skin gets worse after using it, it’s not working-it’s hurting you.
Once you stop, your skin will start healing. But you still need help calming the inflammation.
- Mild cases: Over-the-counter hydrocortisone 1% can help. But if you’re still not better after 5-7 days, you need a stronger option.
- Modest to moderate cases: Prescription corticosteroids like triamcinolone 0.1% or clobetasol 0.05% are first-line. But use them only on thick skin-elbows, knees, palms. Don’t use them on your face, eyelids, or groin. Those areas are thin. High-potency steroids can cause skin thinning in as many as 35% of users after just two weeks.
- Face, eyelids, or sensitive areas: Use low-potency steroids like desonide or switch to non-steroid options like pimecrolimus (Elidel) or tacrolimus (Protopic). These are calcineurin inhibitors. They work as well as steroids for many people, without the thinning risk. About 60-70% of patients see improvement within two weeks.
- Severe or widespread cases: If more than 20% of your body is affected, you’ll need oral steroids like prednisone. A 2-3 week course, tapered slowly, clears up symptoms in 85% of cases within 24 hours.
One thing to watch: tacrolimus and pimecrolimus can cause a burning sensation when first applied. It’s temporary-usually fades after a few days. But many patients quit too soon because of it. Stick with it. The payoff is worth it.
The Paradox: Steroids That Cause the Problem They Treat
It’s frustrating. You get a rash. Your doctor gives you a steroid cream. You use it. The rash spreads. You think it’s getting worse. So you use more. And it keeps spreading.
This is the steroid paradox. The very thing meant to calm your skin is triggering your immune system. Studies show that 0.5% to 2.2% of people using topical steroids develop an allergy to them. That’s not a small number. It’s common enough that dermatologists now ask: Could this be a steroid allergy? before prescribing.
That’s why the trend is shifting. In facial and skin-fold areas-where skin is thin and sensitive-78% of dermatologists now start with tacrolimus or pimecrolimus instead of steroids. Why? Because long-term steroid use on those areas leads to skin thinning, stretch marks, and broken blood vessels. And if you’re allergic? You’re making it worse.
What Happens If You Don’t Find the Cause?
Chronic contact dermatitis doesn’t just itch. It ruins lives.
Patients on HealthUnlocked report an average of 6 months before they get the right diagnosis. They visit 3 doctors. They try 5 different creams. They stop using everything. They feel hopeless. And the truth? 89% of cases clear up completely within 4 weeks-if you remove the allergen. Without that step, only 32% improve.
Healthcare workers are especially at risk. About 18% of nurses and aides develop contact dermatitis from gloves, antiseptics, or topical meds they use daily. Many don’t realize it’s not just “dry skin.” It’s an allergy. And workplaces rarely accommodate them.
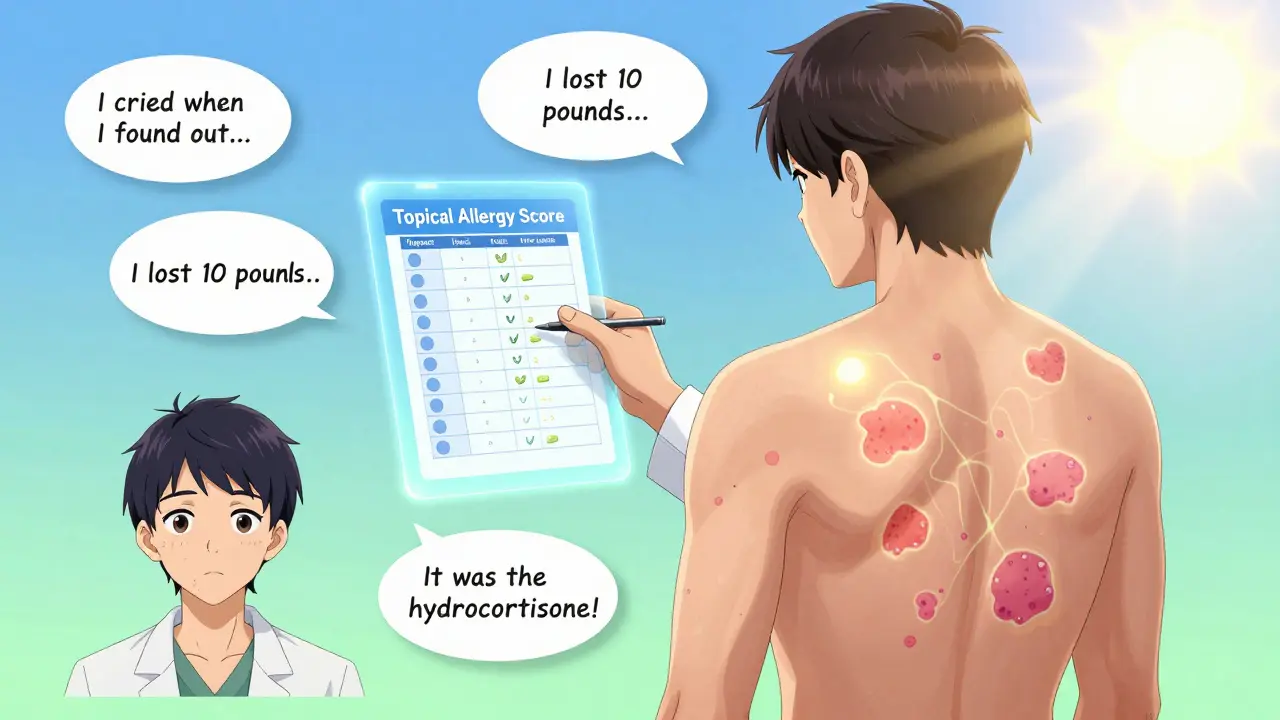
On Reddit, one user wrote: “I used hydrocortisone for my eczema for 3 years. Then my skin started burning. I thought I was getting worse. I kept using it. I lost 10 pounds because I couldn’t sleep. I finally got patch tested. It was the hydrocortisone. I cried when I heard it.”
What’s New in 2026?
Things are changing. Faster than you think.
In 2023, the FDA required all topical prescription labels to list every single ingredient. That’s helped reduce misdiagnosis by 15%. More doctors are now checking the full ingredient list-not just the active drug.
There’s also a new tool: the Topical Medication Allergy Score. Developed in Europe, it’s a checklist doctors use to rate how likely a patient’s rash is caused by a medication. It raised diagnostic accuracy from 65% to 89%.
And research is moving toward prevention. The NIH just funded $4.7 million to study genetic markers that could predict who’s at risk for topical allergies before they even use a cream. Imagine knowing you’re allergic to neomycin before you ever apply it.
Meanwhile, new barrier creams are in Phase 3 trials. They don’t treat the rash-they block allergens from getting into the skin. In tests, they reduced allergen penetration by 73%. That’s huge.
What You Can Do Right Now
If you’ve been struggling with a rash that won’t go away:
- Stop using the cream that seems to make it worse-even if it’s prescribed.
- Write down everything you put on your skin: creams, lotions, sunscreens, even hand sanitizer.
- Make an appointment with a dermatologist who does patch testing. Don’t settle for a general practitioner.
- Ask: “Could this be an allergy to the medicine itself?”
- Use the American Contact Dermatitis Society’s free app to scan products for allergens. It has over 3,500 products listed.
It’s not about avoiding all treatments. It’s about finding the right ones. Your skin doesn’t need more chemicals. It needs the right ones.
Frequently Asked Questions
Can I be allergic to hydrocortisone cream?
Yes. Hydrocortisone is one of the most common causes of topical medication allergies. Even though it’s mild and sold over the counter, about 1 in 50 people develop a delayed allergic reaction to it. If your rash gets worse after using it, stop immediately and get tested.
Is patch testing painful or risky?
No. Patch testing is not painful. Small patches with allergens are taped to your back and left for 48 hours. You might feel slight itching or irritation if you’re allergic, but there’s no needle, no blood, and no serious risk. The only real risk is missing the diagnosis if you don’t get tested.
Can I use steroid creams on my face if I’m not allergic?
Only low-potency ones like desonide, and only for short periods. High-potency steroids like clobetasol can cause skin thinning, stretch marks, and broken capillaries on the face-even if you’re not allergic. For facial rashes, non-steroid options like tacrolimus are safer and just as effective.
Why do some people react to Neosporin and others don’t?
Neosporin contains neomycin, which is a strong allergen. About 10% of people who get patch tested react to it. But not everyone has the immune system that recognizes it as a threat. Genetics, previous exposure, and skin barrier health all play a role. If you’ve used it for years without issue, you’re likely fine. But if you suddenly develop redness or itching after using it, stop and get tested.
How long does it take for contact dermatitis to clear up?
Once you stop the allergen, itching usually improves in 2-3 days. Full healing takes 2-4 weeks. If you keep using the allergen, the rash can last months or become chronic. The key isn’t stronger medicine-it’s stopping the trigger.





Josh McEvoy
January 24, 2026 AT 15:13