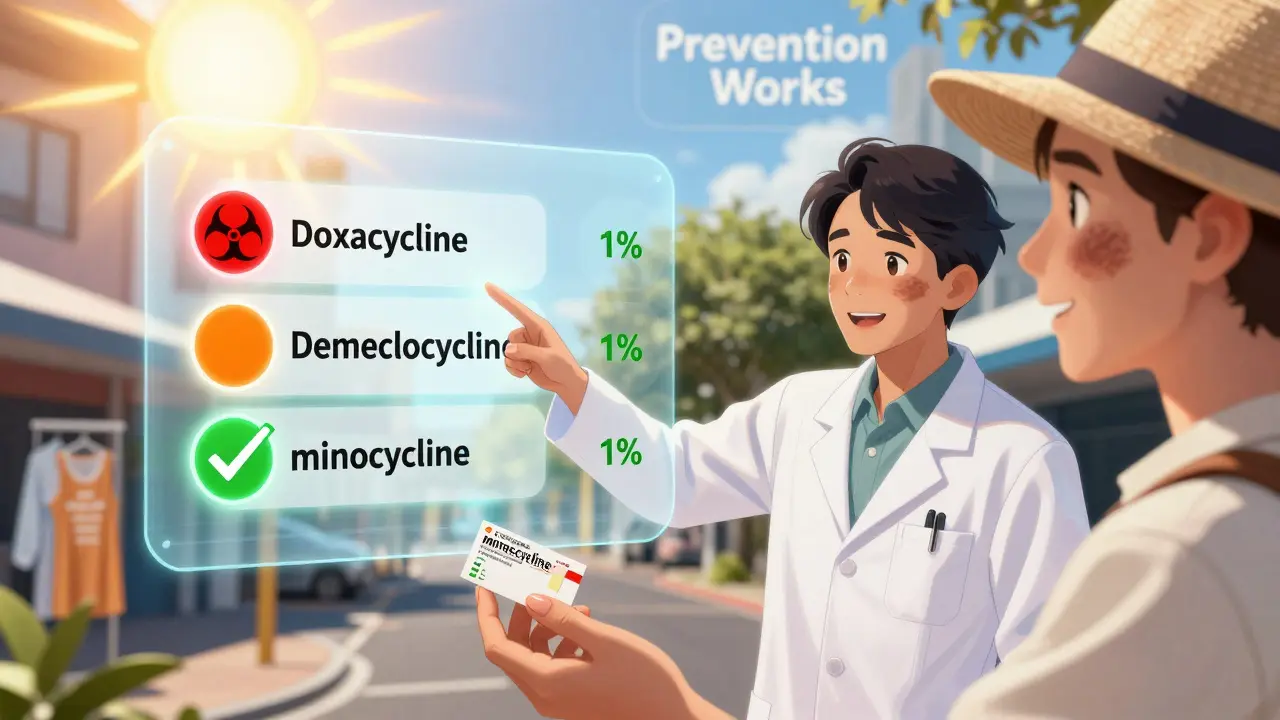
Tetracycline Antibiotic Risk Comparison Tool
How This Tool Works
Select your antibiotic to see its photosensitivity risk level, then compare with alternatives. This tool helps you understand the sun exposure risks associated with your medication and make informed decisions with your doctor.
Antibiotic Comparison
| Antibiotic | Photosensitivity Risk | 30-Day Cost | Common Uses | Protection Needed |
|---|---|---|---|---|
| Doxycycline | 15-42% risk | $30 | Acne, Lyme, pneumonia | High - Daily sun protection essential |
| Demeclocycline | 13-31% risk | $40 | Rarely used | High - Daily sun protection essential |
| Minocycline | <2% risk | $45 | Acne, rosacea | Low - Standard sun protection recommended |
| Sarecycline (Seysara) | 3.2% risk | $550 | Acne | Low - Standard sun protection recommended |
| Omadacycline (Nuzyra) | 2.1% risk | $1,200 | Skin infections | Low - Standard sun protection recommended |
Key Protection Strategies
For Doxycycline Users (High Risk)
Critical Protection Needed
Use mineral sunscreen with zinc oxide as primary ingredient (SPF 50+), wear UPF 50+ clothing, avoid sun exposure between 10am-4pm, and use wide-brimmed hats. These measures reduce risk by over 90%.
Important: Photosensitivity can occur even through windows and on cloudy days. Apply sunscreen 30 minutes before exposure and reapply every 2 hours.
What Tetracycline Photosensitivity Really Means
You’re on tetracycline-maybe for acne, Lyme disease, or a stubborn infection-and suddenly, your skin burns like you’ve been lying on a beach all day… even though you only stepped outside for five minutes. This isn’t bad luck. It’s tetracycline photosensitivity, a well-documented reaction that happens when the antibiotic interacts with UV light. It’s not rare. About 5 to 10% of people taking these drugs get it. And if you’re in a place like Brisbane, where the sun is strong year-round, your risk goes up.
This isn’t an allergy. It’s phototoxicity-meaning the drug itself absorbs sunlight and turns into something that damages your skin. The worst offenders? Doxycycline and demeclocycline. Minocycline? Much safer. The reaction usually shows up as a bad sunburn: red, hot, sometimes blistering. But it doesn’t stop there. You might notice your nails lifting off the nail bed, or dark patches showing up on your face, neck, or arms weeks after you start the medicine. Some people even get tiny, scar-like bumps called milia. These aren’t myths. They’re clinical facts backed by studies from JAMA, the American Academy of Dermatology, and real patient reports.
Why Doxycycline Is the Biggest Culprit
If you’re prescribed doxycycline, you’re getting the most powerful version of tetracycline-but also the one most likely to cause sun damage. Studies show up to 42% of people on high doses (1200 mg/day) develop reactions after UV exposure. Even at the standard 100 mg daily, the risk is real. One 2021 review found that 18.7% of patients on doxycycline reported photosensitivity in online reviews. That’s nearly 1 in 5.
Why? Doxycycline’s molecular structure absorbs UV-A light (320-425 nm), the kind that penetrates deep into your skin-even through windows and clouds. Once it’s activated by sunlight, it generates reactive oxygen molecules that wreck cell membranes, proteins, and DNA. That’s what causes the burn, the blistering, and the long-lasting brown stains. Demeclocycline is almost as bad. But minocycline? Only 2% of users report issues. That’s why dermatologists in Australia and the U.S. are increasingly switching acne patients from doxycycline to minocycline, even if it costs a few dollars more.
It’s Not Just the Beach-Your Daily Routine Is Risky
Most people think they’re safe if they don’t go swimming or sit in direct sunlight. They’re wrong. UV-A rays are everywhere. Driving to work? Your car windows block UV-B but not UV-A. Walking to the mailbox? That’s enough. Sitting near a window at your desk? You’re exposed. A 2022 study showed that 68% of patients who developed severe photosensitivity had no idea their daily habits put them at risk.
One patient in Brisbane posted on Reddit: “I took doxycycline for rosacea. I didn’t go to the beach. But I walked my dog at 8 a.m. and got burned on my cheeks and neck. My doctor never warned me.” That’s the pattern. It’s not about beach days. It’s about cumulative exposure. Even 15 minutes of sunlight can trigger a reaction if you’re on the wrong antibiotic. And once it starts, the damage can linger for months-even after you stop the drug.

How to Protect Yourself-Step by Step
Preventing this isn’t hard. It just takes consistency. Here’s what works, based on dermatology guidelines and real-world success stories:
- Use mineral sunscreen, not chemical. Zinc oxide and titanium dioxide physically block UV-A. Chemical sunscreens (like avobenzone) often don’t cover the full 320-425 nm range. Look for SPF 50+ with zinc as the first active ingredient. CeraVe Mineral SPF 50 and EltaMD UV Clear are top picks.
- Apply enough. Most people use half the amount they need. You need about 2 mg per square centimeter-that’s roughly a shot glass full for your whole body. For your face, use a nickel-sized dollop.
- Reapply every 2 hours. Sweat, water, and rubbing it off reduce protection. Keep a small tube in your bag.
- Wear UPF 50+ clothing. A wide-brimmed hat (at least 3 inches) cuts UV exposure to your face and neck by 73%. Long-sleeved shirts made from sun-protective fabric are game-changers.
- Avoid the sun between 10 a.m. and 4 p.m. That’s when UV-A is strongest, even on cloudy days.
- Install UV-blocking film on your car windows. Standard glass blocks UV-B but lets through 70-80% of UV-A. Aftermarket films block 99%.
One patient on Healthgrades wrote: “I used doxycycline for six months with zero reactions. I wore SPF 50 every day, even indoors. No sunburns. No dark spots. No nail problems.” That’s not luck. That’s protocol.
What About Your Nails?
Photo-onycholysis-nails lifting from the bed-is more common than you think. It happens in 15-20% of people on doxycycline, usually 3 to 6 weeks after starting the drug. It starts with a gap between the nail and skin, often at the tip of one or two fingers. The nail may turn white, yellow, or brown. It’s painless but unsettling. And it doesn’t fix itself quickly. It can take months for the nail to grow out.
There’s no treatment. Prevention is everything. If you notice your nails changing, talk to your doctor. Switching to minocycline or stopping the drug may be needed. Don’t wait. The longer you wait, the more damage accumulates.
Minocycline vs Doxycycline: The Real Choice
Both treat acne, Lyme disease, and respiratory infections. But here’s the breakdown:
| Antibiotic | Phototoxic Risk | Common Use | Cost (30-day supply) |
|---|---|---|---|
| Doxycycline | High (15-42%) | Acne, Lyme, pneumonia | $30 |
| Demeclocycline | High (13/31 in trials) | Rarely used | $40 |
| Minocycline | Low (<2%) | Acne, rosacea | $45 |
| Sarecycline (Seysara) | Very Low (3.2%) | Acne | $550 |
| Omadacycline (Nuzyra) | Low (2.1%) | Skin infections | $1,200 |
If you’re young, active, live in a sunny climate, or spend time outdoors, minocycline is the smarter pick-even if it’s a bit pricier. The cost of treating a bad sunburn, a ruined nail, or long-term pigmentation? Far higher. Primary care doctors often default to doxycycline because it’s cheap. Dermatologists? They know better.
What If You Already Got Burned?
If you’re already reacting-red, swollen, blistered-stop the sun. Immediately. Stay indoors. Cool compresses help. Aloe vera soothes. But don’t pop blisters. That’s how infections start.
See your doctor. You might need a topical steroid to calm inflammation. If your nails are lifting, ask about switching antibiotics. And if you’re still on the drug? Don’t just “be careful.” Be strict. The damage can be permanent. Dark spots from tetracycline photosensitivity can last for years. In some cases, they never fade.
What’s Changing in 2026?
Newer tetracyclines like omadacycline and sarecycline are designed to be less phototoxic. But they cost 10 to 40 times more. Insurance rarely covers them unless you’ve already had a reaction. Meanwhile, researchers are testing “smart” sunscreens with compounds that neutralize tetracycline’s reaction to UV light. Early lab results show up to 70% reduction in damage. That’s promising-but not available yet.
For now, the best tool you have is awareness. And action.
Don’t Let a Prescription Ruin Your Skin
Tetracyclines save lives. But they can also leave lasting marks. The key isn’t avoiding them-it’s using them safely. If your doctor prescribes doxycycline and doesn’t mention sun risk, ask. If they say it’s “rare,” push back. It’s not. It’s common. It’s preventable. And if you’re in Australia, where UV levels are among the highest in the world, you can’t afford to ignore it.
Wear the hat. Apply the sunscreen. Skip the midday walk. Switch to minocycline if you can. Your skin will thank you-not just now, but years from now, when others are wondering why their face still looks sun-damaged.
Can tetracycline cause permanent skin darkening?
Yes. Up to 70% of people who experience tetracycline photosensitivity develop long-lasting hyperpigmentation-brown or gray patches on the face, neck, or arms. These can last months or years, even after stopping the drug. They don’t always fade completely. Prevention is far easier than treatment.
Is minocycline safer than doxycycline for acne?
Yes. Minocycline has less than 2% risk of photosensitivity compared to 15-42% for doxycycline. Both are effective for acne, but minocycline is the preferred choice for people with high sun exposure, outdoor jobs, or a history of sunburns. The slightly higher cost is often worth avoiding long-term skin damage.
Do I need to avoid the sun completely?
No. You don’t need to become a hermit. But you must protect yourself daily. Use SPF 50+ mineral sunscreen, wear UPF clothing, avoid direct sun between 10 a.m. and 4 p.m., and wear a wide-brimmed hat. These steps reduce risk by over 90%. The goal is smart exposure-not total avoidance.
Can sunscreen alone prevent tetracycline photosensitivity?
Not always. Chemical sunscreens often don’t block the full UV-A range (320-425 nm) that triggers the reaction. Mineral sunscreens with zinc oxide or titanium dioxide are more reliable. But sunscreen alone isn’t enough. You also need hats, clothing, and avoiding peak sun hours. Layered protection is key.
Why didn’t my doctor tell me about this?
A 2022 American Academy of Dermatology survey found that 68% of patients who developed photosensitivity were never warned by their provider. Many doctors assume the risk is low or think patients will read the pamphlet. But most don’t. Always ask: “What are the sun risks with this antibiotic?” Don’t assume it’s covered.
How long does photosensitivity last after stopping tetracycline?
The drug clears from your system in 1-2 days, but the skin’s sensitivity can linger for weeks. Some patients report reactions for up to 2 weeks after stopping. Continue sun protection for at least 14 days after your last dose. The pigmentation can last months or longer.
Are there antibiotics that don’t cause sun sensitivity?
Yes. Amoxicillin, azithromycin, and cephalexin have virtually no photosensitivity risk. If you’re on tetracycline and have high sun exposure, ask your doctor if a safer alternative works for your condition. For acne, minocycline is often the best tetracycline option. For infections, other classes may be just as effective.






Donna Macaranas
January 31, 2026 AT 12:20