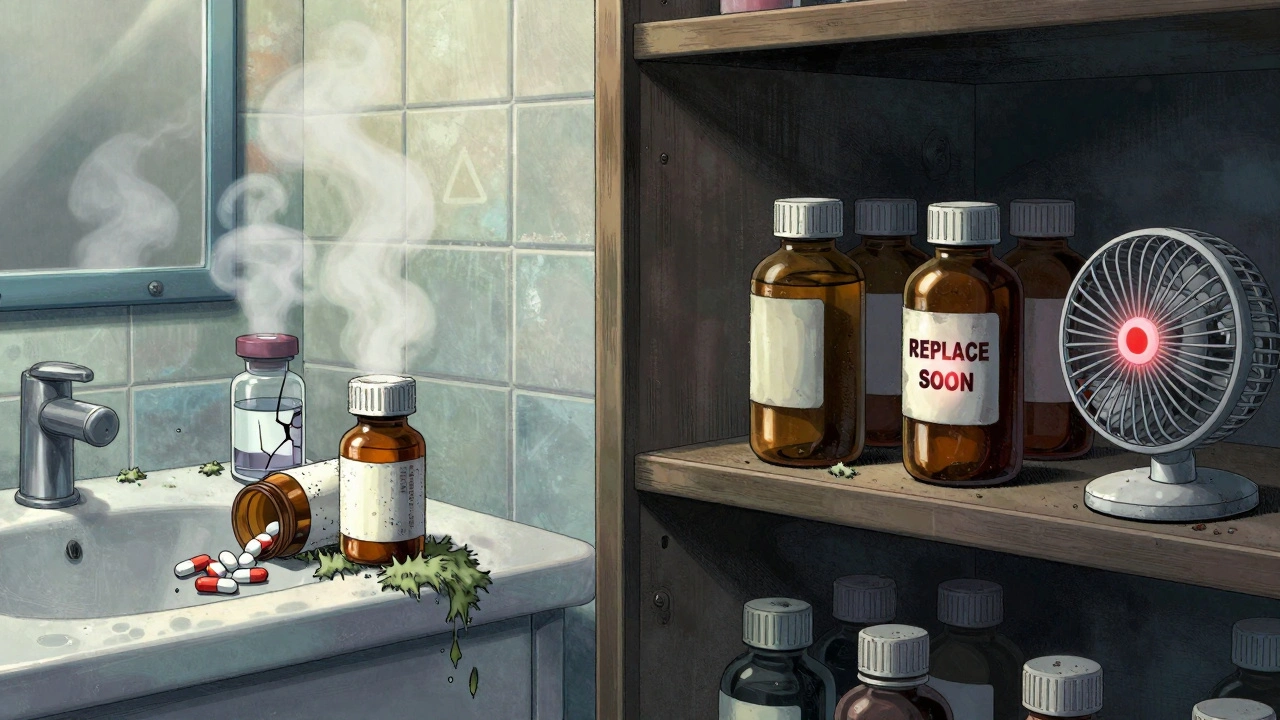
Every year, millions of dollars worth of medications go to waste-not because they’re unused, but because they were stored wrong. You might think your medicine cabinet is safe, but if it’s in the bathroom or near the kitchen stove, you’re risking more than just wasted cash. You’re risking ineffective treatment, dangerous side effects, or even poisoning from degraded drugs. The truth? Most people have no idea how to store their meds properly. And it’s not just about keeping them dry-it’s about temperature, light, packaging, and even where you put them in your house.
Why Medications Expire Sooner Than You Think
Expiration dates aren’t arbitrary. They’re based on strict testing by manufacturers to prove the drug stays at 90-110% of its labeled potency until that date. The FDA requires this. But here’s the catch: those numbers only hold true if the medicine is stored exactly as instructed. If you leave your pills in a steamy bathroom or toss them in a drawer next to a radiator, they can lose effectiveness weeks-or even days-before the printed date.Humidity is the biggest killer of medications. In a typical bathroom, humidity spikes to 85-95% during showers. That’s enough to break down aspirin 300% faster than in dry air. Tablets can absorb moisture, become sticky, crumble, or even grow mold. Liquid medications like eye drops or insulin are even more sensitive. One study found that 78% of expired eye drops became contaminated with bacteria that can cause serious eye infections.
Heat is just as bad. Storing medicine near the stove, oven, or even a sunny window can cause temperature swings of more than 15°C in under 30 minutes. That’s enough to degrade antibiotics, thyroid meds, and even some blood pressure pills within 90 days. And don’t assume your fridge is always safe-putting meds on the door means they’re exposed to warm air every time you open it.
Where NOT to Store Your Medications
- Bathroom cabinets - Steam, humidity, and fluctuating temps make this the worst place in your home. Even if it’s convenient, it’s dangerous.
- Kitchen counters or cabinets near appliances - Heat from the stove, toaster, or microwave can raise the temperature enough to ruin pills and liquids.
- Car glove compartments - In summer, temperatures inside a car can hit 60°C. That’s enough to melt capsules and break down active ingredients.
- Direct sunlight - UV light degrades many drugs. Even clear bottles on a windowsill can cause problems.
- Dresser drawers with no climate control - Unless your room is consistently cool and dry, this isn’t reliable. But it’s still better than the bathroom.
The Right Way to Store Medications
There’s one simple rule: keep meds cool, dry, and dark. The ideal storage temperature is 20-25°C (68-77°F), with humidity below 60%. That’s room temperature in most homes-just not in the bathroom or kitchen.
Use a locked cabinet in a bedroom or closet that’s away from windows and heat sources. If you’re unsure, buy a small digital hygrometer (they cost under $15) and place it near your meds. If the humidity reads above 60%, consider a silica gel packet inside the container (not directly touching the pills).
Always keep medications in their original bottles. Those amber-colored prescription containers block 97% of UV light. Pouring pills into a plastic bag or a pill organizer might seem tidy, but it removes the protective barrier and exposes them to air and light. If you use a pill organizer, only fill it for a week at a time and store it in your cool, dry cabinet-not on the counter.
Special Cases: Insulin, Nitroglycerin, and Other Sensitive Drugs
Some medications need extra care:
- Insulin - Unopened vials must be refrigerated at 2-8°C. Once opened, they can be kept at room temperature (up to 25°C) for up to 28 days. Never freeze insulin. If it looks cloudy, clumpy, or discolored, toss it.
- Nitroglycerin tablets - These are extremely sensitive to light and air. Always keep them in their original dark glass bottle with the cap tightly sealed. Replace them every 3-6 months, even if the expiration date is later.
- Eye drops and liquid antibiotics - Once opened, most last only 28 days. Check the label. If they’re cloudy, have particles, or smell odd, throw them out-even if the date is still good.
- Rectal suppositories and creams - These can melt in heat. Store them in the fridge if your home runs warm, especially in summer.
How to Track Expiration Dates
Most people don’t check expiration dates until they’re out of meds and need a refill. That’s too late. Set up a system.
One proven method: use colored dot stickers. Red = this year, blue = next year, green = two years out. Put one on each bottle. Every month, take five minutes to scan your meds. If you see a red dot, check the date. If it’s expired or close, plan to replace it.
Or assign one person in the household to do a monthly check. Kaiser Permanente found this single habit prevented 89% of unnecessary disposal and 92% of accidental use of expired drugs.
Also, don’t rely on the pharmacy label alone. Some labels list only the fill date, not the expiration. Ask your pharmacist for the manufacturer’s expiration date when you pick up a new prescription.
Signs Your Medication Has Gone Bad
You don’t need a lab test to know if your meds are compromised. Here’s what to look for:
- Tablets or capsules: Discoloration (more than 15% change), cracking, crumbling, sticking together, or a strange odor.
- Aspirin: A strong vinegar smell means it’s broken down into acetic acid. Don’t take it.
- Liquids: Cloudiness, particles, sediment, or a change in color or smell. Eye drops should be clear. If they’re not, throw them out.
- Patches: If they’re brittle, discolored, or no longer stick properly, they’re not delivering the right dose.
If you’re unsure, don’t guess. Take it to your pharmacist. They’ll tell you if it’s safe-or if it’s time to replace it.

What to Do with Expired or Unwanted Medications
Never flush pills down the toilet or throw them in the trash. That’s how drugs end up in our water supply and harm wildlife. In the U.S., 55% of households still do this, according to the CDC.
Use a drug take-back program. The DEA runs National Prescription Drug Take Back Day twice a year. There are over 11,000 permanent collection sites across the country-pharmacies, hospitals, and police stations. Find your nearest one at deas takeback site (note: no links allowed, so just ask your local pharmacy).
If no take-back option is available, mix pills with an unappealing substance like coffee grounds or cat litter, seal them in a container, and throw them in the trash. Remove or black out personal info on the bottle first.
New Tech and Future Improvements
Things are changing. More drug labels now include icons showing storage requirements-like a snowflake for refrigeration or a sun with a slash for avoiding light. Smart pillboxes like the MedMinder Pro now track temperature and humidity and send alerts if your meds are exposed to bad conditions.
Pharmaceutical companies are also developing more stable drugs. Merck’s new heat-stable insulin, approved in late 2023, can last 56 days at 30°C-perfect for hot climates or people without reliable fridges.
And in the next few years, we’ll see prescription bottles with built-in silica gel to keep humidity low. Trials at the University of Wisconsin show these reduce moisture exposure by 45% compared to standard bottles. That could cut expiration rates dramatically, especially in humid areas like Brisbane, where summer humidity regularly hits 80%.
Final Reminder: Your Health Is Worth the Effort
Storing your meds properly doesn’t take much time. It takes a little planning, a little discipline, and a little awareness. But the payoff? Safer, more effective treatment. Less waste. Less risk. And peace of mind.
Next time you reach for a pill, ask yourself: Where did this come from? Is it still good? Is it stored right? If you don’t know the answer, fix it today. Your body will thank you.
Can I still use medication after the expiration date?
The expiration date is the last day the manufacturer guarantees full potency and safety under proper storage. While some studies show certain drugs remain effective years past expiration when stored perfectly (like in military stockpiles), household conditions rarely match that. Humidity, heat, and light degrade drugs faster. For critical medications like insulin, heart pills, or antibiotics, never use expired ones. For occasional pain relievers, if stored well and showing no signs of damage, they may still work-but it’s not worth the risk.
Is it safe to store pills in the fridge?
Only if the label says so. Most tablets and capsules don’t need refrigeration-and in fact, the moisture inside the fridge can damage them. Only refrigerate medications specifically labeled for it, like insulin, some eye drops, or liquid antibiotics. Always keep them in the center of the fridge, not the door, to avoid temperature swings.
Why do some medicines need dark bottles?
Light, especially UV rays, breaks down the chemical structure of many drugs. Amber bottles block 97% of UV light. Medications like nitroglycerin, certain antibiotics, and thyroid pills are especially sensitive. If you transfer them to a clear container, you’re accelerating their breakdown-even if the temperature is perfect.
What’s the best place to store medications in a small apartment?
Choose a high, locked cabinet in a bedroom or hallway, away from windows and heat sources. Avoid the kitchen and bathroom. If you have no cabinet, use a sealed plastic bin with silica gel packs and store it under your bed or on a top shelf. Keep it out of reach of kids and pets. A small digital thermometer and hygrometer can help you confirm the area stays between 20-25°C and below 60% humidity.
Do I need to worry about medications in a hot climate like Brisbane?
Yes, especially in summer. Brisbane’s humidity often exceeds 80%, and indoor temps can climb above 30°C. That’s above the recommended storage range for most drugs. Keep meds in an air-conditioned room, use silica gel, and avoid storing them near windows or in cars. Consider investing in a small climate-controlled medicine box if you take multiple daily medications.





Karandeep Singh
December 2, 2025 AT 10:19