More parents are turning to melatonin to help their kids fall asleep. Between 2007 and 2017, melatonin use among children aged 4 to 17 jumped from 0.5% to 3.1%, according to CDC data. That’s a sixfold increase in just a decade. But just because it’s available over the counter doesn’t mean it’s harmless - especially for kids. Melatonin is a hormone your body naturally makes to signal sleep time. When taken as a supplement, it can help reset a child’s internal clock. But giving it without guidance can backfire - and sometimes dangerously so.
Why Melatonin Isn’t Just a Vitamin
In the U.S., melatonin is sold as a dietary supplement, which means the FDA doesn’t test it for safety, purity, or accuracy before it hits store shelves. A 2022 study in JAMA Network Open found that nearly 70% of melatonin products sold in the U.S. contained significantly more or less melatonin than what was listed on the label. Some had up to 478% more than stated. That’s not a typo. One gummy labeled as 1 mg actually contained almost 5 mg. For a 5-year-old, that’s a massive overdose risk.
In contrast, countries like the U.K. and most of Europe treat melatonin as a prescription-only medication. In those places, it’s regulated like any other drug - meaning dosing is controlled, purity is verified, and it’s only given under medical supervision. The difference in regulation explains why parents in the U.S. are often confused. What they see as a harmless sleep aid is, medically speaking, a hormone-based intervention with real biological effects.
How Much Is Too Much?
Dosing for children isn’t one-size-fits-all. And the range of recommendations across experts is wide - which is why so many parents get it wrong.
- For toddlers and preschoolers (ages 3-5): Start with 0.5 to 1 mg. Some experts say 1 mg is the max, even for this age group.
- For school-age children (6-12): 1 to 3 mg is usually enough. Higher doses (4-5 mg) are sometimes used, but rarely needed.
- For teens (13-18): 1 to 5 mg is typical. Some specialists may go up to 10 mg in rare cases, but only under close supervision.
Here’s the key: melatonin isn’t a sleeping pill. It doesn’t force sleep. It tells the brain it’s time to wind down. Studies show that doses above 1 mg are already higher than what your body naturally produces. A 2024 review in PubMed Central found that even 0.3 mg can mimic your body’s natural melatonin levels. That means most kids don’t need more than 1 mg - and many respond better to even less.
Higher doses don’t mean better sleep. They mean longer-lasting effects - sometimes for more than 24 hours. That can throw off a child’s natural rhythm, leaving them groggy, disoriented, or even nauseated the next day. In rare cases, overdoses have caused vomiting, rapid heartbeat, and low blood pressure. These are medical emergencies.
When and How to Give It
Timing matters just as much as dosage. Melatonin should be given 30 to 60 minutes before bedtime. Giving it too early or too late can confuse the body’s clock instead of helping it. For example, if a child normally goes to bed at 8 p.m., give melatonin at 7:15 p.m. - not right before lights out.
Also, don’t use it as a tool to force compliance. If your child is resisting bedtime because they’re watching TV, playing video games, or drinking soda, melatonin won’t fix that. It’s not a magic fix for poor habits. It’s meant for children whose brains struggle to signal sleep on their own - often due to neurodevelopmental conditions like autism or ADHD.

Who Should Use It - and Who Shouldn’t
Children with autism spectrum disorder (ASD) or attention-deficit/hyperactivity disorder (ADHD) are the most studied group when it comes to melatonin use. For these kids, sleep problems are common - and melatonin can make a real difference. Research shows many children with ASD respond well to low doses over months or even years, under a doctor’s care.
But for healthy kids without diagnosed conditions? The American Academy of Pediatrics (AAP) says there’s not enough long-term data to support routine use. The American Academy of Sleep Medicine (AASM) is even clearer: Behavioral changes should come first. That means consistent bedtimes, no screens an hour before bed, a calm sleep environment, and avoiding caffeine or heavy meals at night.
And children under 3? Most experts agree - don’t use melatonin at all. Sleep issues in toddlers often resolve naturally with routine, daylight exposure, and consistent sleep cues. Melatonin isn’t needed, and the risks outweigh any potential benefit.
What to Look for on the Label
If you do decide to try melatonin, choose products with the USP Verified Mark. That means the manufacturer has been independently tested for accurate dosing and purity. Avoid gummies if you can - they often contain sugar, artificial colors, and inconsistent dosing. Liquid forms or tablets are easier to adjust in small amounts.
Don’t assume that “natural” means safe. Just because melatonin is made in your body doesn’t mean taking extra is harmless. Think of it like giving a child extra insulin - it’s a hormone, and too much can disrupt the system.
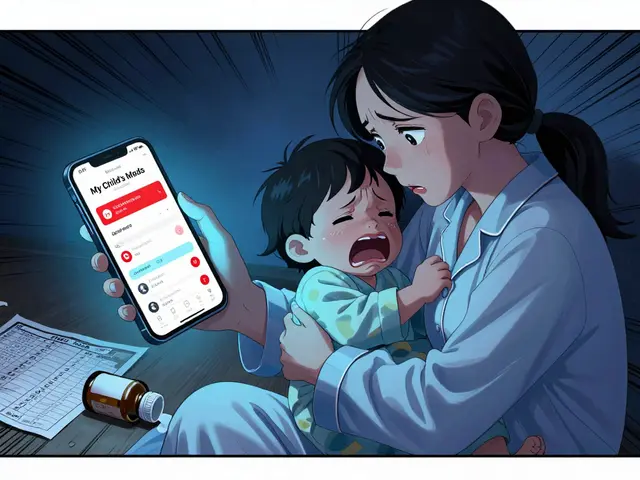
When to Call the Doctor
Always talk to your pediatrician before starting melatonin. They can help rule out other causes of sleep problems - like sleep apnea, anxiety, or even undiagnosed medical conditions. They can also help you pick the right dose and monitor for side effects.
Call your doctor immediately if your child has:
- Vomiting after taking melatonin
- Unusual drowsiness the next day
- Changes in mood, behavior, or appetite
- Signs of an allergic reaction (rash, swelling, trouble breathing)
And if your child’s sleep doesn’t improve after two weeks of consistent use, stop and re-evaluate. Melatonin isn’t a long-term solution for most kids. It’s a temporary tool - not a crutch.
The Bigger Picture: Sleep Hygiene First
Before you reach for melatonin, try these proven, zero-risk steps:
- Set a consistent bedtime and wake-up time - even on weekends.
- Turn off screens at least 60 minutes before bed. Blue light blocks natural melatonin production.
- Keep the bedroom cool, dark, and quiet. Use a white noise machine if needed.
- Avoid caffeine after noon - including soda, chocolate, and energy drinks.
- Establish a calming routine: bath, book, quiet talk - no drama or arguments.
- Get outside in natural light for at least 30 minutes in the morning. This helps regulate the body’s clock.
These steps work. For many families, they’re all that’s needed. Melatonin should be a last resort - not the first step.
What’s Next?
Research on melatonin in children is still evolving. We don’t yet know how long-term use affects puberty, growth, or brain development. That’s why experts urge caution. The rise in use hasn’t been matched by safety data.
If your child is struggling with sleep, don’t panic. Don’t rush to the supplement aisle. Talk to your pediatrician. Start with sleep hygiene. If that doesn’t help, then - and only then - consider melatonin, with clear guidance and a plan to wean off if possible.
Good sleep is one of the most powerful tools for a child’s health - but forcing it with a supplement isn’t the answer. Patience, routine, and professional advice are.
Is melatonin safe for toddlers?
Most pediatricians advise against melatonin for children under age 3. Sleep issues at this age are often caused by developmental changes, teething, or inconsistent routines - not a lack of melatonin. These problems usually improve with better sleep habits, not supplements. Giving melatonin too early may interfere with the child’s natural hormone development.
Can melatonin cause dependency in kids?
Melatonin doesn’t cause physical dependence like prescription sleep meds. But if a child comes to rely on it every night, they may struggle to fall asleep without it. That’s why experts recommend using it for short periods - typically no longer than two to three weeks - unless treating a chronic condition like autism. Always plan a way to wean off under medical supervision.
Why do some kids need higher doses?
Children with autism, ADHD, or other neurodevelopmental disorders often have disrupted natural melatonin production. For these kids, higher doses (up to 5-10 mg) may be needed to help reset their sleep cycle. But even then, doctors start low and increase slowly. Higher doses aren’t better - they’re just necessary for specific medical needs.
Are gummy melatonin supplements safe for children?
Gummies are popular, but they’re risky. Many contain inaccurate doses, added sugar, artificial colors, and flavorings. A 2022 study found that gummy melatonin products often have up to 50% more melatonin than labeled. If you use gummies, choose only those with the USP Verified Mark and check the exact dose per gummy. Liquid or tablet forms are more reliable.
Can melatonin affect puberty or growth?
There’s no strong evidence yet that melatonin affects puberty or growth in children. But because it’s a hormone, experts are cautious. Long-term studies in kids are still lacking. For now, the recommendation is to use the lowest effective dose for the shortest time possible - especially in younger children.
What if melatonin doesn’t work?
If melatonin doesn’t help after 1-2 weeks, stop using it. The problem may not be melatonin deficiency - it could be anxiety, poor sleep habits, an undiagnosed medical issue like sleep apnea, or even too much screen time. Talk to your pediatrician. They may suggest a sleep study or behavioral therapy, which are often more effective than supplements.





Nishant Desae
December 16, 2025 AT 18:36