Getting the right dose of medicine for a child isn’t just tricky-it’s life-or-death. A wrong number, a mix-up between pounds and kilograms, or a missed dose can turn a simple illness into a medical emergency. Pediatric medications aren’t just smaller versions of adult ones. They’re calculated by weight, age, and sometimes even body surface area. One wrong decimal point, and you’re looking at a 300% overdose. That’s not hypothetical. It’s happened. And it’s why tracking pediatric doses with apps and dosing charts isn’t optional anymore-it’s essential.
Why Manual Dosing Is a Recipe for Error
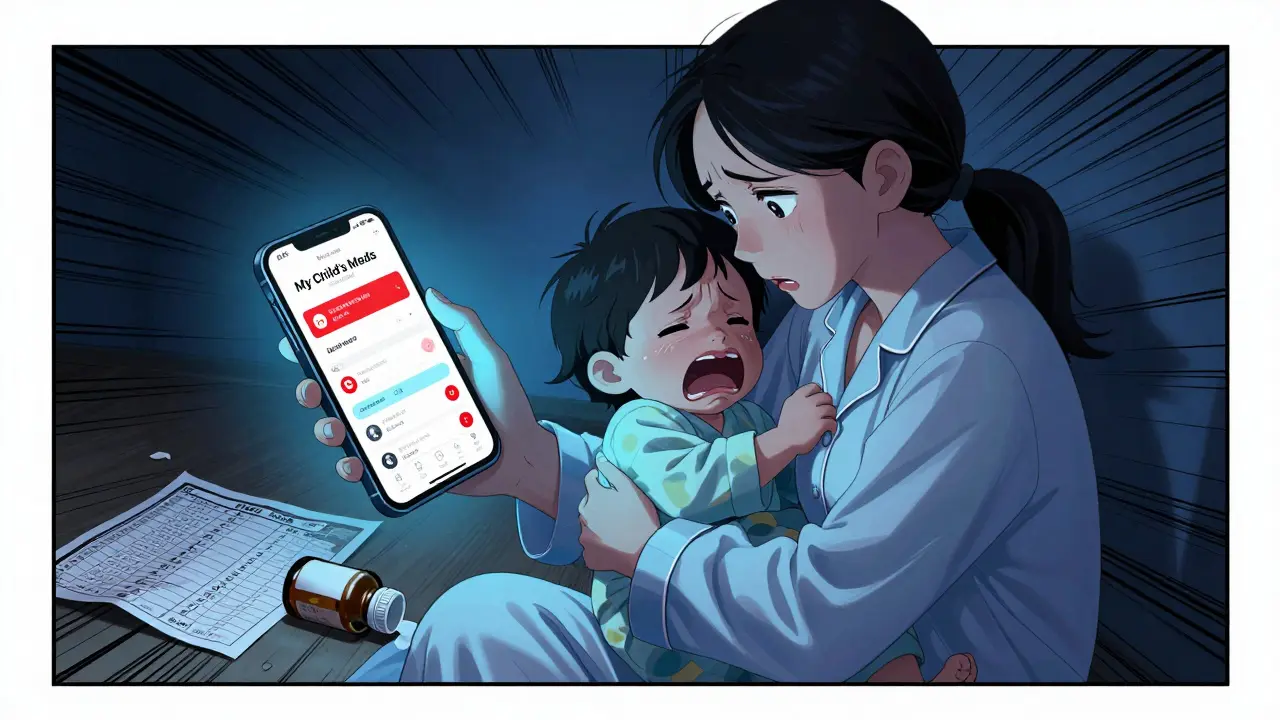
Think back to the last time you had to calculate a dose for your child. You grab the bottle, check the label, find the weight on the chart, do the math, and hope you didn’t mess up. Now imagine doing that at 3 a.m. with a screaming toddler, a half-dead phone, and no coffee. That’s when mistakes happen. Studies show pediatric medication errors occur up to three times more often than in adults. Why? Because the math is harder. A 12-pound baby needs a different amount than a 60-pound child. The same drug, same bottle, wildly different doses. Paper charts? They’re outdated. You’re squinting at tiny print, flipping pages, hoping the chart matches your child’s weight. And if the weight is listed in pounds but the chart uses kilograms? You’re already off. A 2022 study in Pediatric Emergency Care found that manual calculations took an average of 18.7 seconds-and had a 12.3% error rate. That’s more than one in ten doses wrong. In an emergency, that’s not a mistake. It’s a catastrophe.Professional Apps: The Clinician’s Lifeline
In hospitals and ERs, tools like Pedi STAT and Epocrates are standard. These aren’t fancy gadgets. They’re medical devices. Pedi STAT, developed by emergency doctors in Connecticut, lets you type in a child’s weight in kilograms (or pounds-it converts automatically), tap a drug, and get the exact dose for epinephrine, antibiotics, or pain relief in under three seconds. It’s built for speed and accuracy in chaos. Epocrates, around since 1998, has a database of over 4,500 pediatric medications. It doesn’t just give you the dose-it checks for dangerous drug interactions. If you’re about to give acetaminophen and a cold medicine that already contains it? The app warns you. That’s the kind of safety net you want in a busy ER. These apps aren’t free. Epocrates Plus costs $175 a year. Pedi STAT is free, but only for licensed clinicians. They’re designed for professionals who need to make split-second decisions. And they work. A 2023 NIH study showed these tools cut calculation time by 67% and reduced dosage errors by 43% compared to paper. But here’s the catch: these apps don’t talk to your home system. If your child is discharged from the hospital with a new antibiotic, the dose in the hospital’s app doesn’t sync to your phone. That gap? That’s where things go wrong.Parent Apps: Simplicity for the Home Front
At home, you don’t need a complex medical database. You need reminders, clear visuals, and a way to avoid double-dosing. My Child’s Meds is the most trusted app for parents. Developed with input from the Royal College of Paediatrics and Child Health and WellChild, it’s designed like a calendar for medicine. Add your child’s medications, set the times, and the app sends a push notification when it’s time. Missed a dose? It logs it. Accidentally tapped twice? It flags a possible double dose. Parents report a 38% drop in dosing errors using this app. One mom in Brisbane, Sarah K., shared in a verified review: “This app saved us from a potential overdose when my toddler’s fever reducer schedule got confusing during night feedings.” That’s not marketing fluff. That’s real life. Another option, NP Peds MD, gives you simple, pediatrician-approved dosage charts by weight. No calculations. Just look up your child’s weight, find the drug, and you’re done. It’s perfect for over-the-counter meds like ibuprofen or acetaminophen. Consumer Reports found 78% of parents using this app gave the right dose-compared to just 52% using printed charts. But not all apps are created equal. Some, like Child Medical History, are just digital notebooks. They track when you gave medicine but can’t calculate anything. That’s like having a GPS that only shows your location but never tells you how to get where you’re going.
The Big Problem: No One Talks to Each Other
Here’s the hidden danger: your hospital’s app and your home app don’t talk. A child gets discharged with a new prescription. The doctor writes it down. The nurse gives you a paper sheet. You enter it into My Child’s Meds. But the hospital’s Pedi STAT system? It doesn’t export that data. You’re left guessing if the dose matches. A 2023 American Academy of Pediatrics survey found that 87% of medication errors in kids happen during transitions-like going from hospital to home. That’s not the parent’s fault. It’s a system failure. Even worse, some parents download random apps from Google Play that promise “free pediatric dosing.” One case documented in the Journal of Pediatric Pharmacology and Therapeutics involved a 22-month-old who got 300% too much ibuprofen because the app assumed the weight was in pounds, not kilograms. The parent didn’t know the difference. The app didn’t warn them. And there was no safety net.How to Use These Tools the Right Way
Apps aren’t magic. They’re tools. And tools need to be used correctly.- Always double-check the weight unit. Kilograms or pounds? Make sure your app is set right. Most errors happen here.
- Verify with a second source. If the app says 5 mL, check the bottle label. Cross-reference with a trusted chart like the Harriet Lane Handbook (used in hospitals).
- Use paper backups. Power outages happen. Phones die. Keep a printed copy of the dosing schedule in your wallet or fridge.
- Don’t trust unverified apps. If it’s not made by a hospital, pharmacy, or recognized health group, don’t use it for dosing. Stick to apps with clinical backing.
- Reconcile weekly. Compare what’s in your app with your pharmacy’s records. A mismatch could mean your child is getting too much-or too little.

What’s Next for Pediatric Dose Tracking
The future is coming fast. Pedi STAT is testing AI that predicts when a parent might make a mistake based on past behavior. Boston Children’s Hospital is trialing smart pill dispensers that only open when it’s time to give medicine. And HIMSS is working on a new standard to let hospital apps share data with parent apps-finally closing that dangerous gap. By 2027, 95% of pediatric doses given in hospitals will be verified digitally. That’s huge. But the real win will be when your child’s home app and hospital system sync automatically. No more manual entry. No more confusion. Just safe, accurate dosing-every time.What You Can Do Today
If you’re a parent:- Download My Child’s Meds (iOS only, free).
- Use NP Peds MD for quick OTC dosing checks.
- Never use a random app without clinical validation.
- Ask your pediatrician: “Do you recommend a specific app for my child’s meds?”
- Use Pedi STAT or Epocrates in clinical settings.
- Recommend My Child’s Meds to families.
- Teach families how to use it-don’t just hand them a paper sheet.






LALITA KUDIYA
January 7, 2026 AT 03:16