Primaquine is a powerful antimalarial drug used to kill the dormant liver stages of Plasmodium vivax and Plasmodium ovale - the types of malaria that can come back months or even years after treatment. But this drug isn’t safe for everyone. One wrong combination with another medication can trigger serious, even life-threatening reactions. If you’re taking primaquine, you need to know exactly what to avoid - not just prescription drugs, but also over-the-counter pills, herbal supplements, and even some foods.
Why primaquine is dangerous with certain drugs
Primaquine works by breaking down into toxic compounds that kill malaria parasites in the liver. But those same compounds can also damage red blood cells - especially in people with a genetic condition called G6PD deficiency. That’s why the biggest risk isn’t just drug interactions, but how those drugs make primaquine’s side effects worse.
Some medications slow down how your body breaks down primaquine, letting it build up to dangerous levels. Others do the opposite - they speed up its breakdown, making it useless. Then there are drugs that hit the same target as primaquine, like other drugs that stress red blood cells. When you mix them, the result isn’t just nausea or dizziness. It’s hemolytic anemia - a sudden crash in red blood cell count that can send you to the ER.
Drugs you must never take with primaquine
Here are the medications that absolutely should not be mixed with primaquine:
- Doxorubicin - a chemotherapy drug. Combining it with primaquine increases the risk of severe anemia. Studies from the Journal of Clinical Oncology show patients on both drugs had 3x higher rates of hemolysis.
- Sulfonamides - like sulfamethoxazole/trimethoprim (Bactrim). These antibiotics act like primaquine in damaging red blood cells. Even a single dose of Bactrim while on primaquine can trigger acute hemolytic crisis in G6PD-deficient people.
- Nitrofurantoin - used for urinary tract infections. This drug also causes oxidative stress in red blood cells. When paired with primaquine, the combined effect can destroy cells faster than your body can replace them.
- Chloroquine - another antimalarial. While both treat malaria, taking them together doesn’t improve results. Instead, it increases the chance of retinal damage and severe low blood cell counts.
- Probenecid - used for gout. It blocks the kidneys from clearing primaquine, causing the drug to linger in your system longer than intended. This raises the risk of toxicity even in people without G6PD deficiency.
Over-the-counter meds and supplements to skip
You might think OTC drugs are safe, but that’s not true with primaquine.
- Aspirin - even low-dose aspirin can increase bleeding risk when combined with primaquine, especially if you’re already anemic.
- Acetaminophen (Tylenol) - while generally safer than NSAIDs, high doses (over 3,000 mg/day) can stress the liver, which is already working hard to process primaquine.
- Vitamin K supplements - these can interfere with primaquine’s mechanism in the liver. Don’t take them unless your doctor says so.
- Herbal remedies like goldenseal, black cohosh, or kava - these are known to cause oxidative stress. They’re not regulated, so you don’t know how much active ingredient they contain. One capsule could be enough to trigger hemolysis.
What about malaria prevention drugs?
If you’re traveling to a malaria zone, you might be considering other prevention options. Don’t assume they’re interchangeable.
Primaquine is often used as a terminal prophylaxis - taken after returning home to prevent relapse. But if you took atovaquone/proguanil (Malarone) or doxycycline during your trip, you can still safely take primaquine afterward. These drugs don’t interact with primaquine.
However, if you took chloroquine or hydroxychloroquine during your trip, you should wait at least 14 days before starting primaquine. The overlap increases the chance of retinal toxicity and bone marrow suppression.
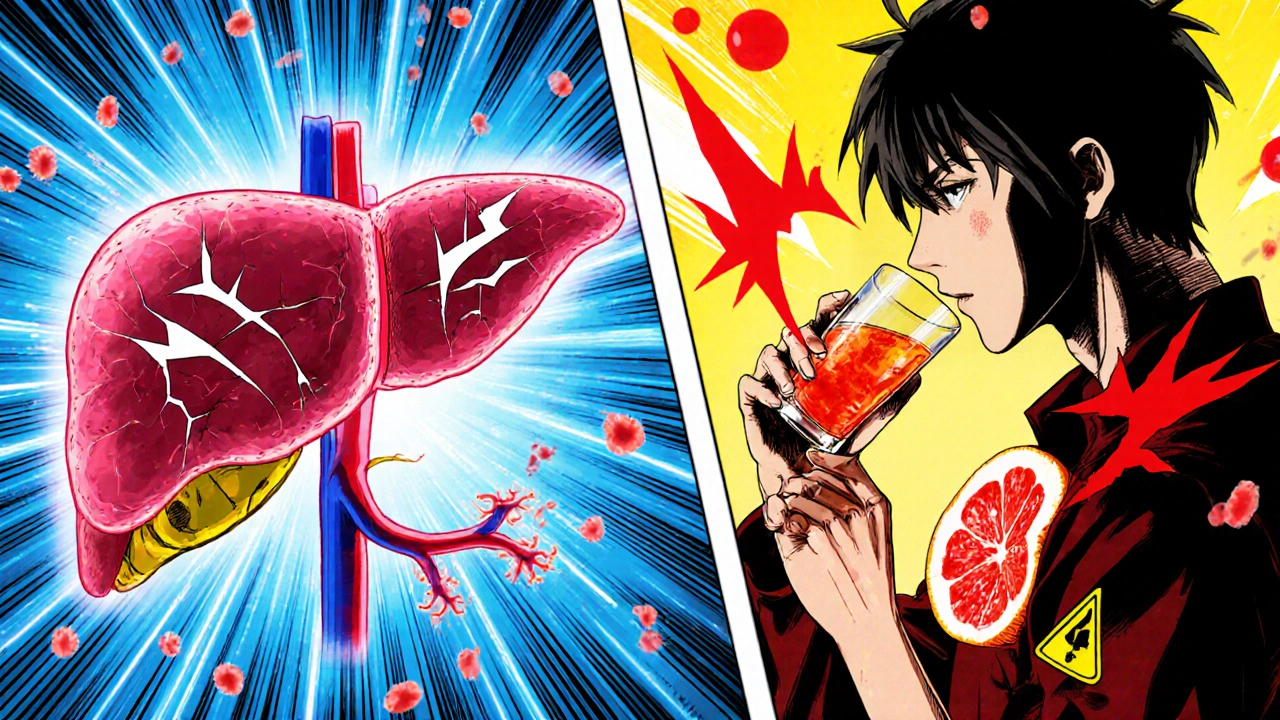
Food and alcohol: what’s safe?
Primaquine doesn’t react with most foods. But alcohol? That’s a different story.
Drinking while on primaquine doesn’t cause direct chemical interactions. But alcohol puts extra strain on your liver - the same organ that’s busy metabolizing primaquine. If you’re already at risk for hemolysis, alcohol can make your body less able to recover from red blood cell damage.
Also, avoid grapefruit juice. It blocks enzymes in your liver that help clear primaquine. Even one glass a day can raise drug levels by 30% or more, pushing you into toxic territory.
What if you have G6PD deficiency?
Over 400 million people worldwide have G6PD deficiency - it’s the most common human enzyme deficiency. In many African, Mediterranean, and Southeast Asian populations, up to 20% of people carry the gene.
If you have it, primaquine can be deadly. You’ll need a blood test before starting treatment. If your G6PD level is below 30% of normal, primaquine is contraindicated. Your doctor will switch you to tafenoquine - a newer drug that’s safer for some G6PD-deficient patients, but still requires testing.
Don’t assume you’re safe just because you’ve never had symptoms. Many people with mild G6PD deficiency never have a problem until they take primaquine or another oxidative drug.

What to do if you accidentally took a bad combo
If you took a drug that interacts with primaquine - even once - watch for these signs:
- Sudden fatigue or weakness
- Dark urine (like cola or tea)
- Yellowing of the skin or eyes
- Rapid heartbeat or shortness of breath
- Fever or chills
These are signs of hemolytic anemia. Stop primaquine immediately and go to the emergency room. Don’t wait. Hemolysis can escalate within hours.
Doctors will check your hemoglobin, reticulocyte count, and bilirubin levels. Treatment usually means IV fluids, oxygen, and sometimes a blood transfusion. The sooner you act, the better your chances.
How to stay safe long-term
Before starting primaquine, tell your doctor about every medication you take - even if you haven’t used it in months. Include:
- Prescription drugs
- OTC painkillers and cold meds
- Vitamins and herbal supplements
- Recent vaccinations
- Any past reactions to drugs
Keep a printed list in your wallet. If you’re hospitalized or see a new doctor, hand it to them. Many ERs don’t know about primaquine interactions - and you can’t rely on their systems to catch it.
Also, get tested for G6PD deficiency if you’re from a high-risk region - even if you’ve never been treated for malaria. It’s a simple blood test. Knowing your status saves lives.
When is primaquine the right choice?
Primaquine isn’t the first-line drug for treating active malaria. It’s used after the main infection is cleared - to prevent relapse. If you’ve been diagnosed with P. vivax or P. ovale, and you’re not pregnant or G6PD-deficient, it’s often the only drug that can stop the parasite from coming back.
But it’s not for everyone. If you’re pregnant, have severe liver disease, or are on other high-risk drugs, your doctor will choose alternatives like weekly chloroquine for 6-12 months. It’s slower, but safer.
Primaquine is powerful. But it’s not a magic bullet. It’s a tool - and like any tool, it can hurt you if you use it wrong.
Can I take ibuprofen with primaquine?
It’s generally safe to take ibuprofen with primaquine in standard doses (200-400 mg every 6-8 hours). But if you’re already anemic or have kidney issues, NSAIDs like ibuprofen can worsen those conditions. Always check with your doctor first, especially if you’re taking primaquine for more than a week.
Is primaquine safe if I have anemia?
No. If you already have anemia - whether from iron deficiency, chronic disease, or another cause - primaquine can make it much worse. It destroys red blood cells, which your body can’t replace fast enough. Your doctor will delay primaquine until your hemoglobin is stable, or choose a different treatment.
Can I drink alcohol while taking primaquine?
It’s not recommended. Alcohol stresses your liver, which is already processing primaquine. It can also mask early signs of hemolysis, like fatigue or dizziness. Even moderate drinking increases your risk of complications. Avoid alcohol entirely while on primaquine and for at least 2 weeks after your last dose.
Does primaquine interact with birth control pills?
There’s no direct interaction between primaquine and hormonal birth control. But if you develop hemolytic anemia from a bad combo with another drug, your body’s ability to absorb or metabolize hormones can change. That could reduce birth control effectiveness. Use backup contraception during and for one month after primaquine treatment.
How long should I wait after stopping another drug before starting primaquine?
It depends on the drug. For sulfonamides or nitrofurantoin, wait at least 7 days. For doxorubicin or probenecid, wait 2 weeks or more. Always ask your doctor - they’ll check how long the other drug stays in your system based on your kidney and liver function.
Can I take primaquine if I’m breastfeeding?
Primaquine passes into breast milk in small amounts. If your baby has G6PD deficiency, it could cause hemolytic anemia. Before taking primaquine while breastfeeding, your baby must be tested for G6PD. If the baby’s status is unknown, avoid primaquine and use an alternative like weekly chloroquine.
If you’re taking primaquine, treat it like a precision tool - not a casual pill. One wrong interaction can turn a simple treatment into an emergency. Know your meds. Know your history. And never assume something is safe just because it’s over-the-counter or natural.







Ifeoluwa James Falola
October 28, 2025 AT 23:37