SGLT2 Inhibitor Bone Risk Checker
Personal Risk Assessment
This tool helps you understand your fracture risk based on the SGLT2 inhibitor you're taking and your personal health factors.
When you're managing type 2 diabetes, choosing the right medication isn't just about lowering blood sugar. It’s about balancing benefits with hidden risks-like bone fractures. SGLT2 inhibitors, a popular class of diabetes drugs, have been praised for protecting the heart and kidneys. But for years, one question has lingered: do they make your bones weaker?
Why Bone Health Matters with Diabetes Drugs
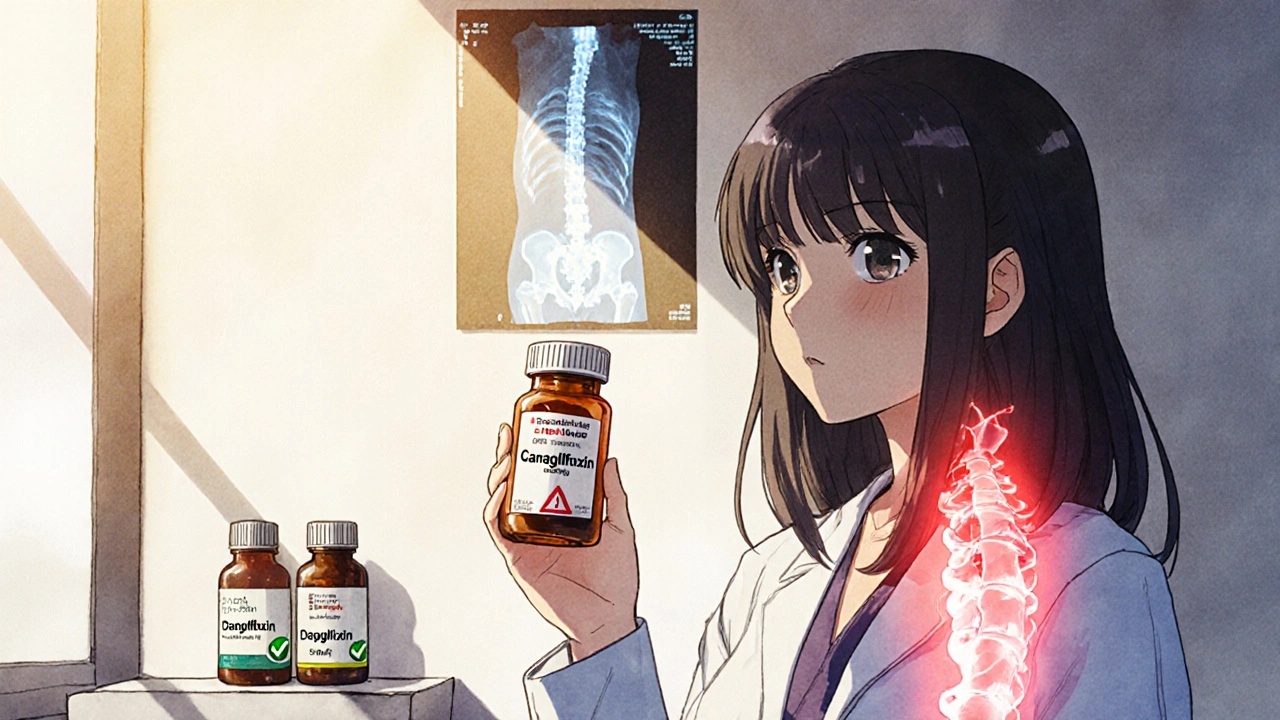
People with type 2 diabetes already have a higher risk of breaking bones, even without taking any meds. High blood sugar damages collagen in bones, reduces muscle strength, and increases fall risk. So when a new drug comes along, it’s natural to wonder: is it making things worse? The first red flag came in 2015. The CANVAS trial, a major study on canagliflozin (brand name Invokana), showed a 26% higher chance of fractures compared to placebo. Most of these breaks happened after minor falls-like slipping on a wet floor or tripping over a rug. The FDA responded with a warning in 2016, and doctors started thinking twice before prescribing canagliflozin to older patients or those with osteoporosis. But here’s where it gets messy: not all SGLT2 inhibitors are the same.Not All SGLT2 Inhibitors Are Created Equal
There are three main SGLT2 inhibitors used today: canagliflozin, empagliflozin (Jardiance), and dapagliflozin (Farxiga). They all work the same way-by making your kidneys dump sugar into your urine. But their effects on bone health? Totally different. Canagliflozin is the only one with consistent fracture risk data. In a two-year FDA-mandated trial, patients on canagliflozin lost 0.92% more bone density at the hip and 1.04% more at the spine than those on placebo. That’s not a huge drop, but in someone already at risk, it’s enough to matter. Empagliflozin and dapagliflozin? No such signal. The EMPA-REG OUTCOME trial (over 7,000 patients) and DECLARE-TIMI 58 (over 17,000 patients) showed no increase in fractures. A 2023 meta-analysis of 27 studies involving nearly 21,000 people found the overall fracture risk with SGLT2 inhibitors was essentially the same as placebo-1.02 times higher, which isn’t statistically meaningful. The FDA still lists a fracture warning for canagliflozin, but not for the others. The European Medicines Agency warns about the whole class, but even they don’t single out specific drugs. Real-world data backs this up: prescriptions for canagliflozin dropped 22% in the U.S. between 2017 and 2022, while empagliflozin and dapagliflozin rose by over 40%.How Could These Drugs Affect Your Bones?
Science doesn’t have all the answers yet, but here’s what we think is happening:- Weight loss: SGLT2 inhibitors help you lose 2-4 kg on average. Less body weight means less mechanical stress on bones-which sounds good, but your body responds by breaking down bone faster to recycle minerals. Studies show this explains only about 3% of bone density changes.
- Phosphate shifts: These drugs make your kidneys hold onto more phosphate. That triggers hormones like FGF23 and PTH, which can pull calcium out of your bones. This effect is stronger with canagliflozin.
- Hormone changes: Women on canagliflozin 300 mg showed a 9.2% drop in estradiol, a key hormone for bone strength. That’s similar to what happens after menopause.
- Falls, not fractures: SGLT2 inhibitors can cause dizziness or low blood pressure when standing up. That increases fall risk-and falls cause fractures. This isn’t a bone problem. It’s a balance problem.

Who Should Be Careful?
You don’t need to avoid SGLT2 inhibitors altogether. But if you’re in one of these groups, talk to your doctor before starting canagliflozin:- You’ve had a fracture before, especially after a minor fall
- You have osteoporosis (T-score ≤ -2.5 on a DXA scan)
- You’re over 70 and have multiple health problems
- You’re a postmenopausal woman with low estrogen
- You take other meds that make you dizzy or weak
What Do Doctors Actually Do?
A 2022 survey of 347 endocrinologists showed how this plays out in real life:- 82% avoid canagliflozin in patients with osteoporosis
- Only 34% do the same for dapagliflozin
- 68% adjust prescriptions based on fracture risk
- 63% say patients worry about fractures more than they should

What About Other Diabetes Drugs?
It’s easy to assume SGLT2 inhibitors are the problem. But compare them to other common diabetes meds:- GLP-1 agonists (like semaglutide): No fracture risk signal. Some studies suggest they might even help bone density.
- DPP-4 inhibitors (like sitagliptin): Neutral. No clear benefit or harm.
- Insulin: Higher fall risk due to hypoglycemia, and it’s linked to lower bone density over time.
What Should You Do?
If you’re on an SGLT2 inhibitor and worried:- Find out which one you’re taking. Is it canagliflozin, empagliflozin, or dapagliflozin?
- If you’re on canagliflozin and have risk factors for fractures, ask your doctor about a DXA scan. It’s a quick, painless X-ray that measures bone density.
- If you’re on empagliflozin or dapagliflozin and have no history of fractures or osteoporosis, you likely don’t need extra testing.
- Focus on fall prevention: remove rugs, install grab bars, get your vision checked, and consider vitamin D and calcium if your levels are low.
- Don’t stop your medication without talking to your doctor. The heart and kidney benefits of these drugs are real and often life-saving.
The Big Picture
The fear around SGLT2 inhibitors and bones was real-but it was mostly about one drug: canagliflozin. And even then, the risk is small and mostly applies to people who are already vulnerable. The American Diabetes Association’s 2023 guidelines say it clearly: SGLT2 inhibitors as a class don’t increase fracture risk. But canagliflozin might, especially at the 300 mg dose in older adults with weak bones. The evidence keeps getting stronger that empagliflozin and dapagliflozin are safe for bones. If you need a powerful diabetes drug with heart and kidney benefits, and you’re not at high fracture risk, you don’t need to avoid them. What matters most isn’t the drug class-it’s your individual risk. Talk to your doctor. Get the right tests. Make an informed choice. Your bones, your heart, and your future self will thank you.Do SGLT2 inhibitors cause bone fractures?
Not all of them. Canagliflozin has been linked to a modest increase in fracture risk, especially in older adults or those with osteoporosis. Empagliflozin and dapagliflozin have not shown this risk in large studies. The overall class does not appear to increase fracture risk for most people.
Which SGLT2 inhibitor is safest for bones?
Empagliflozin (Jardiance) and dapagliflozin (Farxiga) are considered safer for bone health based on current evidence. Canagliflozin (Invokana) carries a specific FDA warning for fractures and should be avoided in people with osteoporosis or prior fractures.
Should I get a bone density scan before starting an SGLT2 inhibitor?
If you’re considering canagliflozin and have risk factors-like being over 70, having had a fracture, or a T-score below -2.0 on a DXA scan-yes. For empagliflozin or dapagliflozin, routine scanning isn’t needed unless you have other reasons to check your bone health.
Can I switch from canagliflozin to another SGLT2 inhibitor?
Yes, if you’re concerned about bone health and are on canagliflozin, switching to empagliflozin or dapagliflozin is a reasonable option. Both have similar blood sugar control and heart/kidney benefits with no increased fracture risk. Talk to your doctor about the switch.
Do SGLT2 inhibitors affect bone density in everyone?
No. Bone density loss was only seen in clinical trials with canagliflozin, and even then, it was small-about 1% over two years. Most people, especially those on empagliflozin or dapagliflozin, don’t experience measurable bone loss. The effect is not universal and depends on the specific drug and individual risk factors.





Skye Hamilton
November 27, 2025 AT 22:44