Vaginal Yeast Infection Treatment Selector
Find Your Best Treatment Option
Answer these quick questions to determine the most appropriate treatment for your vaginal yeast infection. Based on your answers, we'll provide a personalized recommendation.
When a vaginal yeast infection strikes, the first thing most people look for is a quick, reliable cure. Gyne-Lotrimin (the brand name for the imidazole antifungal) is a common go‑to, but it’s far from the only option on the market. Below we break down how Gyne-Lotrimin stacks up against the most popular alternatives, so you can decide which remedy fits your needs best.
What Is Gyne-Lotrimin (Imidazole)?
Gyne-Lotrimin is a topical antifungal medication whose active ingredient is imidazole. Imidazole works by disrupting the cell membrane of Candida yeast, causing the fungus to leak essential nutrients and die. In clinical trials, a single 3‑day course cleared symptoms in about 85‑90% of women.
How Imidazole Differs From Other Antifungals
Most over‑the‑counter (OTC) antifungals belong to the azole family (clotrimazole, miconazole, tioconazole). While imidazole shares the same basic mechanism-blocking ergosterol synthesis-it has a slightly different chemical structure that can affect absorption, irritation potential, and resistance patterns. In practice, those differences translate into nuances in dosing schedules and side‑effect profiles.
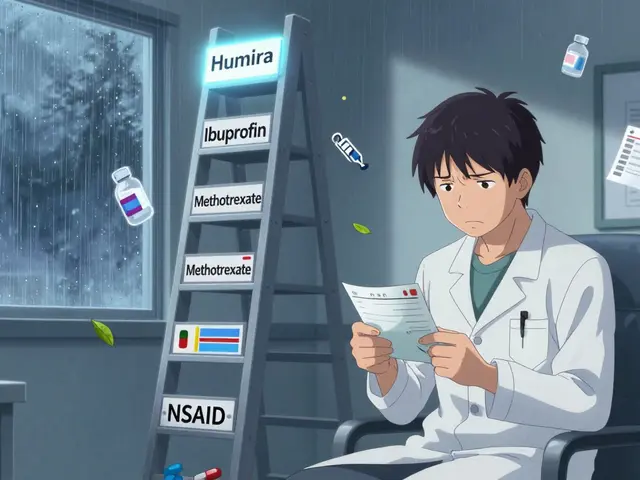
Top Alternatives on the Market
Below is a quick snapshot of the most widely used treatments for vaginal candidiasis.
- Clotrimazole - 1% cream or 2% tablet, typically 7‑day regimen.
- Miconazole - 2% cream, 7‑day or single‑dose option.
- Tioconazole - 6‑hour single dose, 2% ointment.
- Fluconazole - oral tablet, 150 mg single dose (prescription).
- Boric Acid - vaginal suppository, 600 mg nightly for 14 days (alternative for recurrent cases).
- Tea Tree Oil - natural essential oil, used in diluted creams or suppositories (DIY).
- Probiotic Vaginal Suppositories - lactobacillus strains, daily for up to 30 days (prevention focus).

Side‑by‑Side Comparison Table
| Product | Active Ingredient | Formulation | Typical Dosage | OTC / Prescription | Clinical Cure Rate |
|---|---|---|---|---|---|
| Gyne‑Lotrimin | Imidazole | Cream 1% | One applicator nightly for 3 days | OTC (Australia, US) | 85‑90 % |
| Clotrimazole | Clotrimazole | Cream 1% / Tablet 500 mg | 1‑2 g intravaginally for 7 days | OTC | 80‑85 % |
| Miconazole | Miconazole nitrate | Cream 2% | 1 g nightly for 7 days or single‑dose 2 g | OTC | 82‑88 % |
| Tioconazole | Tioconazole | Ointment 6 % | Single dose, 5 g intravaginally | OTC in some markets | 78‑84 % |
| Fluconazole | Fluconazole | Oral tablet 150 mg | Single oral dose | Prescription (US), OTC in some countries | 90‑95 % |
| Boric Acid | Boric Acid | Vaginal suppository 600 mg | Nightly for 14 days | OTC (compounded) | 70‑80 % (refractory cases) |
| Tea Tree Oil | Melaleuca alternifolia oil | Diluted cream or suppository | Applied twice daily for 7‑10 days | OTC (natural) | Variable, ~60‑70 % in small trials |
| Probiotic Suppositories | Lactobacillus spp. | Suppository 10⁹ CFU | Daily for 30 days | OTC (health stores) | Prevention, 30‑40 % reduction in recurrence |
Pros and Cons - Quick Reference
- Gyne‑Lotrimin (Imidazole):
- Pros - short 3‑day regimen, low systemic absorption, widely available.
- Cons - slightly lower cure rate than oral fluconazole, occasional local irritation.
- Clotrimazole:
- Pros - flexible cream or tablet, familiar brand.
- Cons - longer 7‑day course, may cause itching during treatment.
- Miconazole:
- Pros - single‑dose option for busy schedules.
- Cons - higher cost for the single‑dose pack.
- Tioconazole:
- Pros - truly one‑shot treatment.
- Cons - availability limited in some regions.
- Fluconazole:
- Pros - highest cure rates, works systemically for hard‑to‑reach infections.
- Cons - requires prescription in many countries, not ideal for pregnant women without doctor approval.
- Boric Acid:
- Pros - effective for recurrent infections where azoles fail.
- Cons - can cause vaginal dryness, must be used under guidance.
- Tea Tree Oil:
- Pros - natural, pleasant scent, useful for mild cases.
- Cons - limited clinical data, risk of allergic reactions.
- Probiotic Suppositories:
- Pros - helps restore healthy flora, safe for most users.
- Cons - not a cure‑on‑its‑own, best used as adjunct therapy.
Choosing the Right Treatment for You
Here’s a quick decision‑tree you can run through before you head to the pharmacy:
- Is this your first episode? If yes, a short‑course azole like Gyne‑Lotrimin or a single‑dose Miconazole works well.
- Do you need a faster finish because of travel or a special event? Tioconazole’s one‑shot or Miconazole’s single dose save time.
- Are you pregnant or breastfeeding? Talk to your GP-most azoles are considered safe, but oral fluconazole should be avoided unless absolutely necessary.
- Have you had multiple recurrences in the last six months? Consider a 14‑day boric acid regimen or add probiotic suppositories after the antifungal course.
- Do you prefer a natural approach? Diluted tea tree oil may soothe mild symptoms, but keep an eye on irritation.
When in doubt, a quick chat with a pharmacist can confirm whether a particular brand is stocked locally and whether you need a prescription.
Safety Tips and When to Seek Medical Help
- Stop any product that causes severe burning, swelling, or rash-those are signs of an allergic reaction.
- If symptoms linger beyond 7 days despite treatment, it could be a resistant strain or a different infection (bacterial vaginosis, STI). See a doctor.
- Women with diabetes, HIV, or weakened immune systems often need a longer or more aggressive regimen; oral fluconazole is a common choice.
- Never use products intended for external use (like regular skin antifungal creams) inside the vagina; they can disrupt the natural pH.
Frequently Asked Questions
Can I use Gyne‑Lotrimin while pregnant?
Imidazole is classified as Category B in the US, meaning animal studies show no risk but there aren’t enough human studies. Most clinicians consider short‑term use acceptable, but you should always check with your obstetrician first.
How does the cure rate of Gyne‑Lotrimin compare to oral fluconazole?
Fluconazole’s single‑dose regimen typically clears 90‑95 % of cases, slightly higher than Gyne‑Lotrimin’s 85‑90 %. The difference matters most for stubborn or recurrent infections where systemic treatment reaches deeper tissue.
Is boric acid safe for long‑term use?
Boric acid is safe for short courses (usually 14 days). Prolonged daily use can cause vaginal dryness and, in rare cases, systemic absorption issues. Use it only under medical guidance.
Do probiotic suppositories replace antifungal medication?
No. Probiotics help rebalance the vaginal microbiome after an infection, but they don’t kill the yeast directly. Pair them with an antifungal for the best results.
Can I mix tea tree oil with Gyne‑Lotrimin?
Mixing them isn’t recommended. Both can irritate the mucosa, and the combined effect isn’t studied. Choose one method and stop if you notice worsening discomfort.




parbat parbatzapada
October 21, 2025 AT 12:20