Azathioprine Dosage Calculator
Recommended Azathioprine Dosage Calculator
This tool helps determine the appropriate starting dose of azathioprine based on your TPMT enzyme activity level, as recommended by major medical guidelines. Always consult your healthcare provider before starting any new medication.
Recommended Dosage
Select your TPMT activity level and click 'Calculate Recommended Dosage' to see your results.
Monitoring Recommendations
Your monitoring requirements will appear here based on your TPMT level.
Important: This calculator provides general guidelines based on medical literature. Your specific situation may require adjustments from your healthcare provider. TPMT testing does not replace regular blood monitoring while on azathioprine.
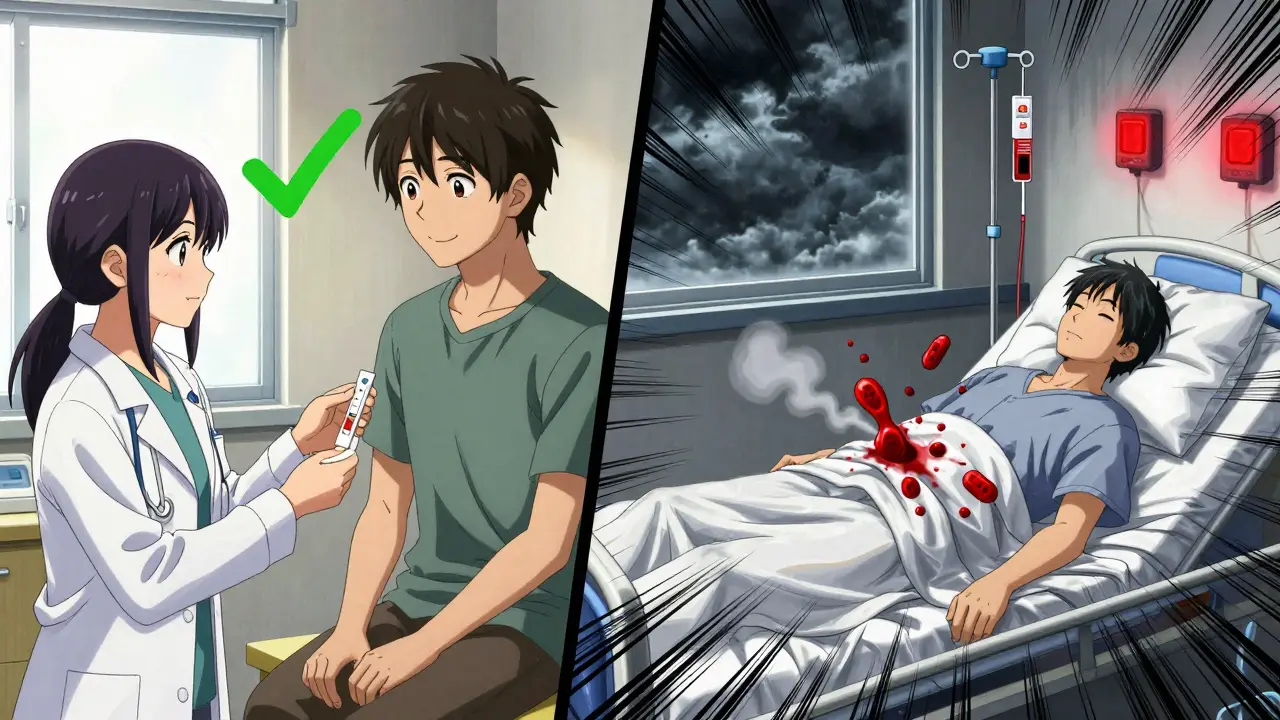
When you’re prescribed azathioprine for Crohn’s disease, lupus, or after a kidney transplant, your doctor isn’t just giving you a pill-they’re handing you a drug with a hidden risk. For most people, it works fine. But for a small group, it can crash their blood cell counts so hard they end up in the hospital with infections, bleeding, or worse. The good news? There’s a simple test-TPMT testing-that can spot those at risk before the first dose is even taken.
What Azathioprine Does and Why It’s Risky
Azathioprine has been around since the 1960s. It’s cheap-often under $50 a month-and it works. It shuts down parts of the immune system that attack your own body in autoimmune diseases or reject a transplanted organ. But it doesn’t just target the bad actors. It hits fast-dividing cells everywhere, including the bone marrow where your blood cells are made.
That’s where things get dangerous. About 15% to 28% of people on azathioprine have side effects. Nausea is common and usually mild. But in 1 in 300 people, something much worse happens: their bone marrow stops making enough white blood cells, red blood cells, or platelets. This is called myelosuppression. Without enough white cells, you can’t fight infections. Low platelets mean you bleed easily. It can kill.
Why does this happen in some and not others? It’s not random. It’s genetics.
TPMT: The Enzyme That Keeps You Safe
Your body breaks down azathioprine using an enzyme called thiopurine methyltransferase, or TPMT. Think of TPMT as a safety valve. It turns the active parts of the drug into harmless waste so they don’t pile up and poison your bone marrow.
Some people are born with gene variants that make their TPMT enzyme weak or completely inactive. If you have two bad copies of the gene (homozygous), you have almost no TPMT activity. That’s rare-only about 0.3% of people. But if you have one bad copy (heterozygous), your enzyme works at about half speed. That’s about 10% of the population.
Here’s the key: if you’re homozygous and you take a normal dose of azathioprine, your body can’t clear it fast enough. The drug builds up. Your bone marrow gets crushed. Studies show these patients have a 90% chance of severe, life-threatening low blood counts within weeks.
For heterozygous people, the risk is lower-but still real. Most doctors reduce their dose by 30% to 70% to stay safe. But without testing, you’re just guessing.
What TPMT Testing Actually Tells You
TPMT testing isn’t a blood test you get at your local clinic. It’s a genetic test. A cheek swab or blood sample is sent to a lab that looks for specific gene changes-like *2, *3A, *3B, and *3C-that tell you how your TPMT enzyme will behave.
There’s also a phenotyping test that measures enzyme activity directly in your red blood cells. But it’s unreliable if you’ve had a blood transfusion recently. Genotyping is the gold standard.
Results come back in 3 to 7 days. They’ll say one of three things:
- Normal activity: You can start at the full dose (1.5-2.5 mg/kg/day) with routine blood monitoring.
- Intermediate activity: Start at 30-70% of the normal dose. Check your blood counts weekly for the first month.
- Low or absent activity: Do NOT take azathioprine. Switch to something else-like methotrexate or a biologic.
That last one is critical. If you’re homozygous deficient, azathioprine is a death sentence at standard doses. No exceptions.
But TPMT Isn’t the Whole Story
Here’s where things get messy. Not everyone who gets sick on azathioprine has a bad TPMT gene.
In one study of 139 patients, only 1 out of 13 who had to stop the drug because of side effects had low TPMT activity. The rest? Their liver got damaged, their pancreas inflamed, or they got a weird skin rash. None of those were linked to TPMT.
And then there’s NUDT15-a second gene that’s just as important, especially for people of Asian descent. Up to 20% of East Asian populations carry variants that make them super sensitive to azathioprine. In fact, in some groups, NUDT15 defects cause more toxicity than TPMT. That’s why guidelines now say: test for both.
Even more complicated: drugs like allopurinol (used for gout) block the same enzyme pathway as azathioprine. If you’re on both, your TPMT status doesn’t matter-you’re still at high risk. Your doctor needs to know every medication you’re taking.
And let’s not forget: even if your genes are fine, you still need regular blood tests. TPMT testing doesn’t replace CBCs. It just helps you start safer.
What the Guidelines Say
The American Gastroenterological Association (AGA), the European Crohn’s and Colitis Organisation (ECCO), and the Clinical Pharmacogenetics Implementation Consortium (CPIC) all agree: test before you start.
But they don’t all agree on how hard to push it. The AGA says testing is recommended. ECCO says it’s recommended but not mandatory. Why the hesitation? Cost and evidence.
A 2011 trial with 333 patients found that routine TPMT testing didn’t reduce the overall number of side effects. The rate was 28% with testing and 29% without. That’s because most side effects aren’t caused by TPMT-they’re caused by other things. But the trial did catch the one patient who was homozygous deficient. That one person was saved from near-certain disaster.
So the real value isn’t in preventing every side effect. It’s in preventing the ones that kill.
Cost vs. Benefit
Azathioprine costs $20-$50 a month. A biologic like infliximab costs $1,500-$2,500 per infusion. So it’s tempting to skip the test and save money.
But here’s what the hidden cost looks like: if you develop severe myelosuppression, you’re looking at hospitalization, antibiotics, blood transfusions, and maybe weeks off work. That single hospital stay can cost $15,000-$30,000. The TPMT test? $200-$400.
Insurance usually covers it. In the U.S., most commercial plans pay. In Australia, it’s often covered under Medicare if ordered by a specialist. The real barrier isn’t cost-it’s awareness. Many community doctors still don’t order it.

What to Do If You’re Prescribed Azathioprine
If your doctor prescribes azathioprine, ask these three questions:
- Have you ordered TPMT and NUDT15 testing before I start?
- If I have intermediate or low activity, what will my starting dose be?
- What blood tests will I need, and how often?
Don’t be afraid to push back if they say, “We’ve never done that before.” This isn’t experimental. It’s standard of care in most major hospitals. If they’re not doing it, they’re not following current guidelines.
While you wait for results, don’t panic. You can start low-dose azathioprine in some cases if you’re under close monitoring. But if your test comes back homozygous deficient, stop. Don’t wait. Switch to methotrexate or another agent. There are options.
Real Stories, Real Risks
One patient in Brisbane, diagnosed with ulcerative colitis, had her TPMT test done before starting azathioprine. Her result showed intermediate activity. Her doctor cut her dose in half. Six months later, her blood counts were stable. Her friend, who skipped the test, started at full dose. Three weeks in, her white blood cell count dropped to 1.2 (normal is 4-11). She ended up in the ER with a fever and pneumonia. She had to stop azathioprine for good.
Another patient in Melbourne had normal TPMT but developed severe liver damage. He didn’t know until his bilirubin shot up. His doctor told him: “Your genes were fine, but your body reacted badly.” That’s the truth. Genetics help, but they don’t guarantee safety.
And yes, some people get nausea. It’s common. It often fades. But if you’re dizzy, pale, or have unexplained bruises or fevers-get your blood checked. Now.
What’s Next?
The field is moving fast. More labs now offer multi-gene panels that test TPMT, NUDT15, and even glutathione-S-transferase variants in one go. Companies like OneOme and GeneSight are making it easier for doctors to order these tests.
The FDA updated azathioprine’s label in 2019 to include warnings about both TPMT and NUDT15. That’s a big deal. It means the drug maker acknowledges the risk.
But the biggest change? The mindset. We’re no longer just treating diseases-we’re tailoring treatment to your DNA. Azathioprine is one of the clearest examples of how pharmacogenomics saves lives. It’s not science fiction. It’s happening now.
Don’t let cost, convenience, or old habits keep you from asking the right questions. Your bone marrow doesn’t care if the test is expensive or “not routine.” It only cares if you give it a dose it can’t handle.
Is TPMT testing mandatory before taking azathioprine?
No, it’s not legally mandatory, but it’s strongly recommended by major medical groups like the AGA and CPIC. Many hospitals and specialists require it. Skipping it puts you at risk of severe, avoidable side effects-especially if you have low TPMT activity.
Can I take azathioprine if my TPMT test shows low activity?
No. If your TPMT activity is severely low or absent, azathioprine can cause life-threatening bone marrow failure. You should not take it. Your doctor will switch you to another immunosuppressant like methotrexate or a biologic.
Does TPMT testing guarantee I won’t have side effects?
No. TPMT testing only predicts risk for myelosuppression caused by poor drug metabolism. It doesn’t protect against liver damage, pancreatitis, or allergic reactions. You still need regular blood tests and to report any new symptoms to your doctor.
What if I’m Asian? Do I still need TPMT testing?
Yes-but you also need NUDT15 testing. In Asian populations, NUDT15 gene variants are a bigger cause of azathioprine toxicity than TPMT. Many labs now test both genes together. If you’re of East Asian, South Asian, or Hispanic descent, ask specifically for NUDT15 screening.
How long does it take to get TPMT test results?
Results usually take 3 to 7 days. Some labs offer faster turnaround. If your condition is urgent, your doctor may start you on a low dose while waiting for results, but only if you’re being closely monitored with weekly blood tests.
Can I get TPMT testing without a doctor’s order?
In most places, no. TPMT testing is a medical test that requires a doctor’s order because the results directly affect your treatment plan. Direct-to-consumer genetic tests like 23andMe don’t include TPMT variants and shouldn’t be used for this purpose.
What if I’ve already been on azathioprine for months without problems?
That’s good-but it doesn’t mean you’re safe forever. Toxicity can develop at any time. If you haven’t had TPMT testing, it’s still worth getting done. It helps your doctor understand your risk profile and adjust your monitoring plan. Some people are lucky and never have side effects. But luck isn’t a treatment plan.







Russ Kelemen
January 31, 2026 AT 08:11