For years, people taking statins have wondered: could these cholesterol-lowering pills be linked to ALS? It’s a scary thought. ALS - also known as Lou Gehrig’s disease - is a devastating condition that slowly steals muscle control, speech, and eventually the ability to breathe. And statins? They’re among the most common drugs in the world, taken by millions to prevent heart attacks and strokes. So when rumors started swirling about a possible connection, it wasn’t just a medical question - it became a personal one for countless patients.
Where Did This Fear Come From?
The concern didn’t come from a lab study or a breakthrough paper. It started with reports. In 2007, the U.S. Food and Drug Administration (FDA) began seeing more spontaneous reports linking statin use to ALS. These weren’t controlled studies - just doctors and patients filing notices when something unusual happened. The FDA took it seriously. By 2008, they reviewed data from 41 large clinical trials involving thousands of people. The result? No increase in ALS cases among those taking statins compared to those on placebo. They made it clear: statins shouldn’t be stopped based on these reports. But the fear didn’t disappear. Why? Because ALS is rare, slow to develop, and hard to study. People diagnosed with ALS often see their doctors for muscle weakness, cramps, or fatigue - symptoms that can also be side effects of statins. So sometimes, patients stop taking statins before they even get an ALS diagnosis. That creates a misleading pattern: statin use looks like it’s happening right before ALS shows up. But it’s not causing it - it’s being stopped because of it.The Science Gets Messy - And That’s Normal
Research since then has gone in all directions. Some studies say one thing. Others say the opposite. That’s not a flaw - it’s how science works. In 2024, a genetic study using Mendelian Randomization claimed that three statins - atorvastatin, simvastatin, and rosuvastatin - might increase ALS risk. The numbers were dramatic: one statin showed an odds ratio over 693,000. That sounds alarming. But experts immediately raised red flags. Genetic studies like this can produce wild results if they don’t account for how genes affect multiple body systems at once (called pleiotropy). Many scientists called the findings implausible. Meanwhile, a much larger, real-world study from Norway looked at 524 ALS patients over decades. They tracked who took statins, when, and for how long - using national health records that don’t miss a beat. Their conclusion? No link to ALS survival. Statin users lived just as long as non-users. The difference in survival time? Less than a month - statistically meaningless. And here’s the twist: that same Norwegian study found that 21% of ALS patients stopped statins in the year before diagnosis. Why? Because their early ALS symptoms - muscle pain, weakness - looked exactly like statin side effects. So they quit. But those who stopped had worse outcomes. Not because statins were harming them. Because stopping statins left them vulnerable to heart problems while ALS was already progressing.Long-Term Use Might Actually Help
One of the most surprising findings came from a 2024 study in Neurology. It showed that people who took statins for more than three years had a lower risk of developing ALS - especially men. That’s the opposite of what the fear suggested. How could that be? Some lab research offers a clue. In mouse models of ALS, certain statins like lovastatin and atorvastatin reduced motor neuron loss by up to 30%. They seemed to calm inflammation in the brain and spinal cord - a key driver of ALS progression. Statins don’t just lower cholesterol. They also reduce inflammation, improve blood flow, and stabilize cell membranes. These effects might be protective in the nervous system. Dr. Marc Weisskopf from Harvard, who co-authored that study, put it plainly: “Long-term statin use had a protective role against the development and progression of ALS.”
What Do the Experts Say Today?
Major medical groups are aligned: statins are not a known cause of ALS. The Mayo Clinic updated its patient page in January 2024 with a clear statement: “There’s no good evidence that statins cause or trigger ALS.” The European Medicines Agency reviewed all the data in 2023 and found no causal link. The FDA still stands by its 2008 conclusion: don’t stop statins based on ALS concerns. Even the American Heart Association, which sets the gold standard for heart disease treatment, continues to recommend statins as first-line therapy for high-risk patients. Their guidelines haven’t changed. Dr. Shafeeq Ladha, lead author of the Norwegian study, said it best: “Statin use should not routinely be discontinued upon diagnosis of ALS.”What Should You Do If You’re Taking Statins?
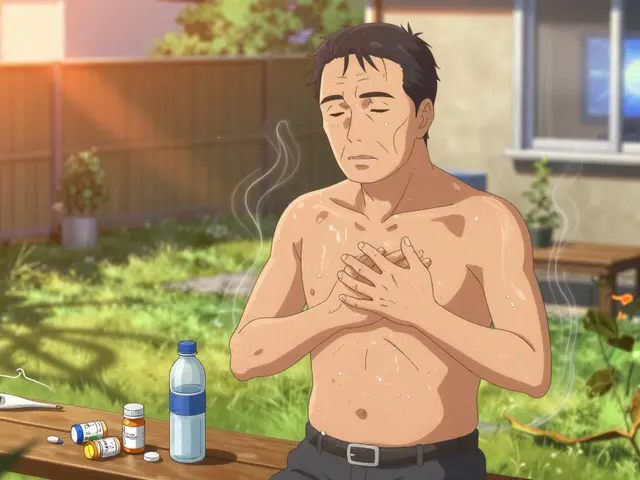
If you’re on a statin and you’re healthy - no ALS symptoms - keep taking it. The benefits for your heart and brain far outweigh any unproven risk. If you’ve been diagnosed with ALS, don’t stop your statin unless your doctor tells you to. Stopping could raise your risk of heart attack or stroke. And if you’re having muscle pain or weakness, don’t assume it’s from the statin. It could be early ALS. That’s why you need a neurologist to evaluate it properly. Many patients stop statins out of fear. One survey found 35% of ALS patients ask about it. Twelve percent actually quit. That’s dangerous. Statins save lives. Don’t trade one risk for another.




Johannah Lavin
November 19, 2025 AT 06:32