Genetic Arrhythmia Syndrome Explorer
This interactive tool helps you understand the major inherited arrhythmia syndromes. Select a condition below to learn more about its genetic basis, clinical features, and treatment strategies.
Long QT Syndrome
(LQT1)
Most common form caused by KCNQ1 mutations
Long QT Syndrome
(LQT3)
Caused by SCN5A mutations, triggered by rest
Brugada Syndrome
SCN5A loss-of-function mutations
CPVT
RYR2 or CASQ2 mutations
Select a Condition to View Details
Click on any card above to explore information about that inherited arrhythmia syndrome.
Key Genes Involved
- KCNQ1 LQT1
- KCNH2 (HERG) LQT2
- SCN5A LQT3, Brugada
- RYR2 CPVT
- CASQ2 CPVT
Treatment Approaches
- Beta-blockers (first-line for LQT1)
- Mexiletine (for LQT3)
- ICD implantation (high-risk Brugada)
- Avoid triggers (fever, certain drugs)
- Lifestyle modifications
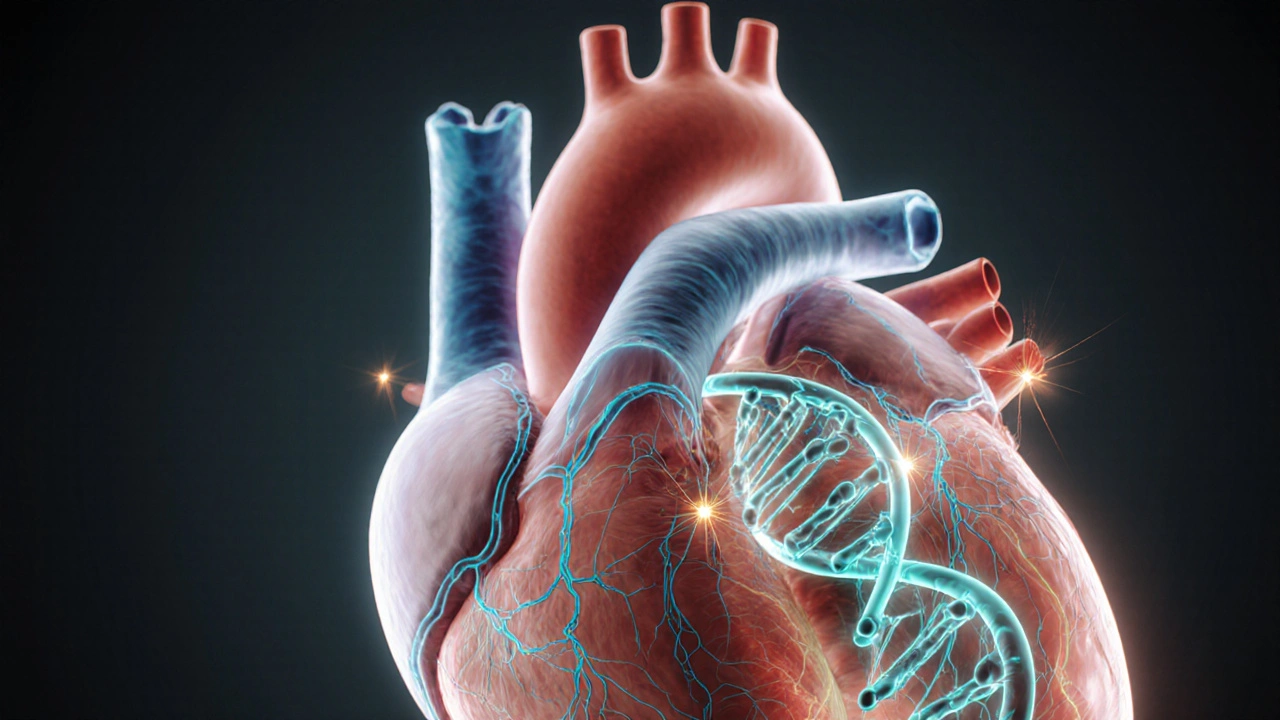
When doctors discuss Genetics the study of DNA variations that influence health and disease, they’re pointing to the blueprint that makes each heart beat a little different. Understanding how that blueprint shapes heart rhythm problems has moved from a niche curiosity to a core part of cardiology practice.
What Exactly Is an Arrhythmia?
An arrhythmia any disturbance in the normal timing or sequence of heartbeats can feel harmless, like an occasional skipped beat, or life‑threatening, like ventricular fibrillation. The most common types - atrial fibrillation, supraventricular tachycardia, and ventricular tachycardia - arise from a mix of electrical, structural, and hormonal factors. Yet a growing slice of these disorders trace back to inherited DNA changes, making genetics a key piece of the puzzle.
How Genetics Drives Rhythm Disorders
At its core, a genetic mutation can alter the proteins that control ion flow across heart cells. If a sodium channel opens too easily or a potassium channel closes too slowly, the electrical wave that tells the heart to contract gets scrambled. Over the last decade, next‑generation sequencing has identified dozens of such culprit genes, turning vague family histories into concrete molecular explanations.
Major Inherited Arrhythmia Syndromes
Three hereditary conditions dominate the discussion because they have clear genetic roots, distinct ECG signatures, and specific treatment pathways.
- Long QT Syndrome a disorder that prolongs the heart’s repolarisation phase, raising the risk of sudden torsades de pointes
- Brugada Syndrome characterised by ST‑segment elevation in right precordial leads and a predisposition to ventricular fibrillation
- Catecholaminergic Polymorphic Ventricular Tachycardia exercise‑ or stress‑triggered ventricular tachycardia without structural heart disease
The genetics behind each syndrome differ, but the clinical stakes are similar - early detection can mean the difference between a routine check‑up and an implantable cardioverter‑defibrillator (ICD).
Key Genes and Their Effects
Below are the most frequently implicated genes, each tied to a specific ion channel or regulatory protein.
- SCN5A encodes the cardiac sodium channel Nav1.5; mutations cause both Long QT Type 3 and Brugada patterns
- KCNQ1 produces the potassium channel Kv7.1; loss‑of‑function variants are the most common cause of Long QT Type 1
- KCNH2 also known as HERG, this gene forms the rapid delayed rectifier potassium channel; mutations lead to Long QT Type 2
- RYR2 codes for the cardiac ryanodine receptor; dysfunctional calcium release underlies CPVT
- CASQ2 encodes calsequestrin, a calcium‑binding protein; rare variants also cause CPVT
Even within a single gene, different mutation types (missense vs. truncating) can produce opposite ECG phenotypes, underscoring the need for precise molecular diagnosis.
Genetic Testing: From Panels to Whole‑Genome Sequencing
Modern cardiac genetics labs offer targeted panels that screen the dozen most relevant genes for a fraction of the cost of whole‑exome sequencing. Results are usually reported as pathogenic, likely pathogenic, variant of uncertain significance (VUS), or benign. A VUS can be frustrating, but family segregation studies and functional assays often re‑classify these over time.
In practice, clinicians follow a stepwise approach:
- Collect a detailed three‑generation pedigree.
- Order a gene panel if the phenotype matches one of the classic syndromes.
- Refer to a genetic counsellor for pre‑ and post‑test discussion.
- Integrate results into risk‑stratification tools (e.g., QT‑dispersion scores, Brugada risk scores).
Because testing can reveal incidental findings (e.g., predisposition to cardiomyopathy), ethical consent is essential.
Emerging Research: GWAS, Polygenic Scores, and Gene Editing
A recent Genome‑Wide Association Study large‑scale analysis linking common DNA variants to disease traits involving over 200,000 participants identified more than 30 loci that modestly influence QT interval length. While each single‑nucleotide polymorphism (SNP) adds only a few milliseconds, together they form a polygenic risk score that predicts who might develop drug‑induced QT prolongation.
Beyond risk prediction, the CRISPR‑Cas9 system is being explored to correct pathogenic SCN5A mutations in induced pluripotent stem‑cell cardiomyocytes. Early models show restored sodium currents and normalized action potentials, hinting at future gene‑therapy options for otherwise untreatable arrhythmias.
These advances translate into two practical messages for today’s patients:
- Even if a single‑gene test is negative, polygenic risk may still inform medication choices.
- Clinical trials are already recruiting for CRISPR‑based interventions, offering a glimpse of personalized, curative therapy.

Clinical Implications: Managing Patients with Genetic Arrhythmias
Knowing the genetic cause reshapes three core aspects of care: risk assessment, family screening, and therapy selection.
- Risk assessment: A pathogenic SCN5A loss‑of‑function mutation in a Brugada patient raises the threshold for ICD implantation compared with a merely symptomatic individual.
- Family screening: First‑degree relatives should undergo ECG and, if indicated, targeted genetic testing. Cascade testing can uncover silent carriers who benefit from lifestyle counseling (e.g., avoiding fever‑inducing medications in Brugada).
- Therapy selection: Beta‑blockers are first‑line for LQT1 (KCNQ1) but may be less effective in LQT3 (SCN5A); mexiletine, a sodium‑channel blocker, is often added for the latter.
Guidelines from the American Heart Association and European Society of Cardiology now recommend integrating genetic data into the decision‑making algorithm for all major inherited arrhythmia syndromes.
Practical Checklist for Patients and Clinicians
- Document any sudden cardiac events in the family, including ages at onset.
- Request a 12‑lead ECG for every at‑risk relative, even if asymptomatic.
- Consider a comprehensive gene panel if the ECG shows prolonged QT, Brugada‑type ST elevation, or exercise‑induced VT.
- Engage a certified genetic counsellor before and after testing.
- Update risk scores annually; new variants and polygenic data may change management.
- Stay informed about ongoing clinical trials (CRISPR, RNA‑based therapies).
By following these steps, patients can move from uncertainty to a clear, evidence‑based care plan.
Key Takeaway
The field of cardiac genetics has shifted from rare case reports to everyday clinical tools. Whether you’re a patient with a family history of sudden death or a physician navigating treatment options, the blend of gene‑specific knowledge, modern testing, and emerging therapies offers a roadmap for safer hearts. genetics isn’t just a buzzword - it’s the lens through which we now understand and prevent many life‑threatening arrhythmias.
| Condition | Key Gene(s) | Inheritance | Typical ECG Finding | Common Trigger | First‑Line Treatment |
|---|---|---|---|---|---|
| Long QT Syndrome (LQT1) | KCNQ1 | Autosomal dominant | QTc > 480ms | Exercise, especially swimming | Beta‑blocker (e.g., nadolol) |
| Long QT Syndrome (LQT3) | SCN5A | Autosomal dominant | Marked QT prolongation, prominent T‑wave | Rest, sleep | Mexiletine + beta‑blocker |
| Brugada Syndrome | SCN5A (loss‑of‑function) | Autosomal dominant | ST elevation in V1‑V3 | Fever, certain drugs | ICD for high‑risk patients |
| Catecholaminergic Polymorphic VT | RYR2, CASQ2 | Autosomal dominant | Normal resting ECG | Exercise or emotional stress | Beta‑blocker (nadolol) ± flecainide |
Frequently Asked Questions
Can lifestyle changes reduce the risk of genetically driven arrhythmias?
Yes. For example, individuals with LQT1 should avoid intense swimming, while those with Brugada syndrome need to keep fever under control and steer clear of sodium‑channel‑blocking drugs. Tailoring activity and medication based on the specific gene mutation can markedly lower event rates.
How reliable are genetic tests for arrhythmias?
Targeted panels have a diagnostic yield of 30‑40% in patients with a clear phenotype. Whole‑exome sequencing can raise that to ~50%, but interpretation becomes more complex. A certified genetic counsellor helps translate results into actionable care.
Is an implantable cardioverter‑defibrillator (ICD) needed for every genetic arrhythmia?
No. ICD implantation is reserved for high‑risk individuals-those with a prior cardiac arrest, sustained ventricular tachycardia, or a very high‑risk genotype (e.g., SCN5A loss‑of‑function with spontaneous Type1 Brugada ECG). Many patients are managed successfully with medication and lifestyle modifications alone.
Can children be tested for these genes?
Yes, especially when a parent carries a pathogenic variant. Early testing allows clinicians to start protective therapies before any symptoms appear, dramatically reducing the chance of sudden cardiac death.
What’s the future of gene therapy for arrhythmias?
Clinical trials using CRISPR‑based editing of SCN5A or RYR2 are entering PhaseI. If safety and efficacy are proven, we could see the first disease‑modifying treatments for inherited rhythm disorders within the next decade.





Brian Johnson
October 8, 2025 AT 14:03