Heat Risk Calculator for Medication Users
Personal Risk Assessment
This calculator helps you understand your heat exposure risk when taking diuretics or anticholinergics. It's based on CDC guidelines and medical research.
Your Heat Risk Assessment
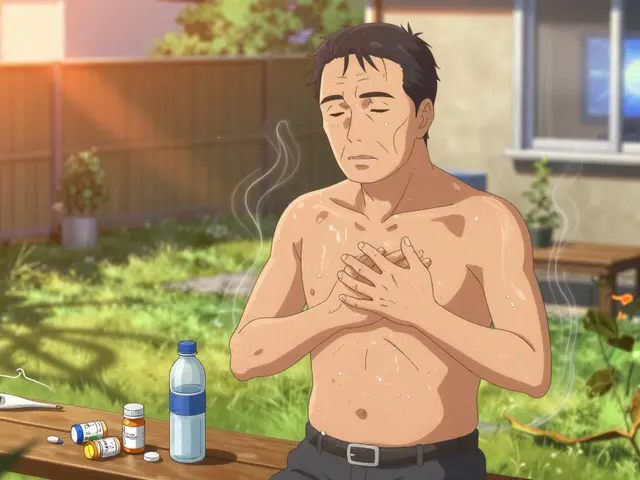
When the temperature climbs, most people think about drinking more water, staying in the shade, or wearing light clothes. But if you're taking diuretics or anticholinergics, those simple steps aren't enough. These medications can turn a hot day into a medical emergency-without you even realizing it.
Why Heat Is Dangerous with These Medications
Diuretics, like furosemide (Lasix) or hydrochlorothiazide (Microzide), make you pee more. That’s how they lower blood pressure and reduce swelling. But when it’s hot, your body needs every drop of fluid to cool itself through sweat. Diuretics strip away water and electrolytes-especially sodium and potassium-right when you need them most. Your blood volume drops. Your heart works harder. Your kidneys struggle to keep up. Even mild dehydration can trigger dizziness, cramps, or worse. Anticholinergics are another silent threat. Medications like oxybutynin (Ditropan), tolterodine (Detrol), or amitriptyline (Elavil) block acetylcholine, a chemical that tells your body to sweat. If you’re on one of these, your sweat glands shut down-by 30% to 50%. That means your body can’t cool itself, even if you’re standing in front of a fan. Your core temperature rises. You don’t feel hot. You don’t feel sweaty. And by the time you feel dizzy or confused, it’s already too late. The CDC lists both drug classes as top contributors to heat-related deaths. In the 2021 Pacific Northwest heat dome, over 60% of those who died from heat had taken either a diuretic or an anticholinergic. And these aren’t rare drugs. Around 32 million Americans take diuretics. Nearly 40% of adults over 65 are on at least one anticholinergic. Many don’t even know they’re at risk.How Your Body Fails in the Heat
Your body has one main way to cool down: sweat. When sweat evaporates, it pulls heat away from your skin. That’s physics. But if you’re on anticholinergics, that mechanism is broken. You don’t sweat enough. Your skin stays dry. Your temperature keeps climbing. You might feel fine-until your brain starts to fog. That’s because anticholinergics also cause confusion, forgetfulness, and drowsiness. Heat illness symptoms like headache, nausea, or disorientation? They look just like side effects of the medication. You might think, “I’m just tired from my pills,” and not realize you’re in danger. Diuretics make things worse. As you lose fluid, your blood thickens. Your heart pumps faster to keep oxygen moving. Your kidneys, already stressed from the drug, can’t hold onto sodium or potassium. Low potassium means muscle weakness or irregular heartbeat. In extreme heat, that can lead to cardiac arrest. Studies show the risk isn’t just during heatwaves. A 2022 study of 1.2 million Medicare patients found that people on loop diuretics had a 37% higher chance of being hospitalized for heat illness-even when temperatures were just 80°F (26.7°C). That’s not a heatwave. That’s a normal summer day in Brisbane, Atlanta, or Phoenix.What You Should Do (Step by Step)
Don’t stop your meds. That’s the first rule. Stopping diuretics or anticholinergics without your doctor’s approval can cause fluid buildup, high blood pressure, or bladder problems. But you can adjust how you live around them.- Drink more water-but don’t overdo it. If you have heart failure, your doctor may have told you to limit fluids. During heat, that rule may need to change. Ask your doctor: “Should I drink more on hot days?” Most will say yes. Sip water all day. Don’t wait until you’re thirsty. Thirst means you’re already dehydrated.
- Watch your electrolytes. Diuretics deplete potassium and magnesium. Eat bananas, spinach, avocados, or nuts. If you’re on long-term diuretics, ask your doctor about a blood test to check your levels. Don’t take potassium supplements unless prescribed.
- Check your sweat. If you’re on an anticholinergic, test your sweat response. Stand in a warm room for 10 minutes. Do you feel damp? Do you see sweat? If not, your body isn’t cooling itself. That’s a red flag.
- Wear the right clothes. Light colors, loose fit, breathable fabric like cotton or linen. Avoid dark, tight, or synthetic materials. They trap heat. Even if you’re not sweating much, airflow helps.
- Use sunscreen. Many anticholinergics make your skin more sensitive to UV rays. Sunburn adds stress to your body. Use SPF 30+ daily, even if you’re just stepping outside.
- Plan your day. Avoid being outside between 10 a.m. and 4 p.m. when the sun is strongest. If you must go out, carry a water bottle, wear a wide-brimmed hat, and find shade every 20 minutes.

Who Should Be Watching Out for You?
This is where many people get hurt. Anticholinergics can make you forgetful. Diuretics can make you weak. Heat makes you confused. You might not realize you’re in trouble. That’s why you need someone else to check on you. The CDC recommends a “buddy system.” Pick one person-a family member, neighbor, or friend-and ask them to call or visit you twice a day during heat alerts. Ask them to look for signs: Are you answering slowly? Are you dry? Are you unusually quiet? Are you not eating or drinking? These aren’t normal aging signs. They’re warning signs. If you live alone, set phone reminders to drink water every hour. Use a smart speaker to ask, “Am I drinking enough?” Some people use wearable thermometers that alert if their core temperature rises above 38°C (100.4°F). These aren’t common yet-but they’re becoming more available.When to Call for Help
Heat illness doesn’t always start with a headache. Sometimes, it starts with silence. If you or someone you know is on these medications and shows any of these signs, call emergency services immediately:- Confusion, slurred speech, or inability to answer simple questions
- Hot, dry skin with no sweat
- Rapid heartbeat or chest pain
- Nausea or vomiting that won’t stop
- Fainting or loss of consciousness

What Doctors Are Doing About It
Doctors know this is a growing problem. In 2022, a pilot study at Massachusetts General Hospital found that 42% of heart failure patients on diuretics needed temporary dose reductions during a July heatwave. That’s not rare. It’s common. Some clinics now use “heat risk scores” for older patients. They look at: age, medications, kidney function, mobility, and living situation. If your score is high, your doctor might adjust your dose, schedule a blood test, or connect you with a community health worker. The National Institute on Aging has invested over $4 million to study how medications affect heat tolerance in seniors. Penn State is running a major trial tracking 500 adults over 60 in real heat conditions. Results will be out in 2025. Until then, the best advice is simple: know your meds. Know your risk. Talk to your doctor before the next heat spell.Final Thought: It’s Not Just About the Weather
Climate change is making heat more frequent, longer, and deadlier. In the U.S., the number of days over 90°F has jumped 47% since 1970. In Australia, Brisbane saw its hottest year on record in 2024. These aren’t isolated events. They’re the new normal. Your medications aren’t the enemy. But they change how your body responds to heat. Ignoring that link is dangerous. You don’t need to live in fear. You just need to be informed. Ask your doctor: “Am I at risk for heat illness?” Write down the answer. Share it with someone. Keep it in your wallet. The next time the temperature spikes, you won’t be caught off guard. You’ll know what to do. And that might save your life.Can I stop taking my diuretic if it’s too hot?
No. Stopping diuretics without medical supervision can cause fluid buildup, worsening heart failure or high blood pressure. Instead, talk to your doctor about adjusting your dose or fluid intake during hot weather. Never make changes on your own.
Do anticholinergics make me more sensitive to the sun?
Yes. Many anticholinergic drugs, including oxybutynin and amitriptyline, increase photosensitivity. This means you can burn more easily and quickly in the sun. Always use broad-spectrum SPF 30+ sunscreen and wear protective clothing, even on cloudy days.
What’s the best way to stay hydrated if I’m on diuretics?
Sip water consistently throughout the day-don’t wait until you’re thirsty. Aim for clear or light yellow urine. Avoid alcohol and caffeine, which can worsen dehydration. If you’re on a fluid restriction due to heart failure, ask your doctor if it’s safe to increase intake during heat. Many will say yes.
How do I know if I’m dehydrated while on these meds?
Dry mouth, dark urine, dizziness, fatigue, and muscle cramps are early signs. But with anticholinergics, you might not sweat-even if you’re dehydrated. Check your skin: if it’s hot and dry instead of damp, that’s a red flag. A simple test: pinch the skin on your forearm. If it doesn’t snap back quickly, you’re likely dehydrated.
Are older adults at higher risk?
Yes. Older adults are more likely to take both diuretics and anticholinergics. Their bodies also cool less efficiently, they feel thirst later, and they may have other conditions like kidney disease or dementia that make heat illness harder to recognize. This combination makes them the most vulnerable group.
Can I still exercise if I’m on these medications?
Yes-but be cautious. Avoid outdoor exercise during peak heat hours. If you exercise indoors, keep the room cool and drink water before, during, and after. Stop immediately if you feel dizzy, nauseous, or unusually tired. Low-intensity activities like walking in the early morning or stretching are safer options.






Elizabeth Alvarez
December 28, 2025 AT 06:14