When your doctor hands you a prescription for a generic drug, do you feel relieved-or skeptical? You’re not alone. Millions of people in the U.S. and around the world take generic medications every day, saving hundreds or even thousands of dollars a year. But behind those savings is a quiet battle: the battle for patient trust. Why do some people refuse generics-even when they’re cheaper and just as effective? And what can doctors, pharmacists, and healthcare systems do to turn doubt into confidence?
What Exactly Is a Generic Medication?
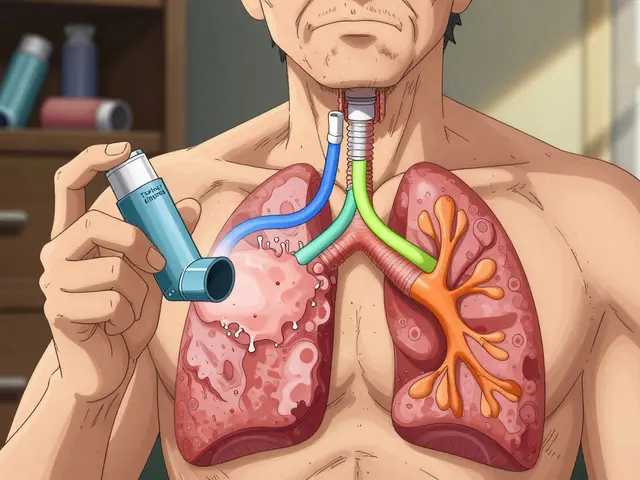
A generic drug isn’t a copy. It’s not a knockoff. It’s the exact same medicine, in the same strength, with the same active ingredient, meant to work the same way as the brand-name version. The FDA requires generics to meet strict bioequivalence standards: they must deliver between 80% and 125% of the active ingredient into the bloodstream at the same rate as the brand-name drug. That’s not close enough-it’s clinically identical. For example, generic metformin works the same as Glucophage. Generic atorvastatin is chemically identical to Lipitor. The only differences? The color, shape, or inactive ingredients like fillers or dyes. Those don’t affect how the drug works. They just make the pill look different. The system was created by the 1984 Hatch-Waxman Act in the U.S., which let generic manufacturers skip expensive clinical trials by proving their version matched the original. Today, 90% of all prescriptions filled in the U.S. are for generics. Yet they make up only 23% of total drug spending. That’s because generics cost 80% to 85% less than brand names.Why Do People Still Doubt Generics?
The biggest barrier isn’t science-it’s perception. In Greece, nearly a third of patients say they’d rather pay more for a brand-name drug because they believe it’s higher quality. In the U.S., that number is lower-only 6% of patients say they distrust generics outright-but the doubts run deeper than that. Many people don’t trust them because they’ve never been properly explained. Here’s what patients actually worry about:- ‘Will it work the same?’-Even though studies show no difference in effectiveness, 24% of patients in one Greek study said they feared generics wouldn’t relieve symptoms as well.
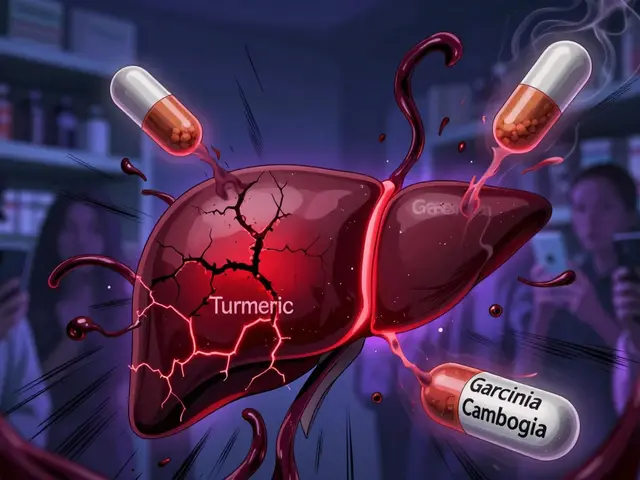
- ‘Will I have side effects?’-29.5% of patients fear new or worse side effects from generics, even though the active ingredient is identical.
- ‘Why does it look different?’-Pill appearance changes every time you refill. One month it’s white, the next it’s blue. That’s not a mistake-it’s normal. But without explanation, it feels like you’re getting a different drug.
- ‘Is this the real thing?’-Some patients think generics contain less active ingredient. The FDA says no. Generics must contain 90-110% of the active ingredient. The myth that they’re only 80% effective is widespread-and wrong.
Who Trusts Generics-and Who Doesn’t?
Trust isn’t random. It follows patterns. Older adults trust generics more. People over 60 are 71% more likely to believe generics are safe than younger patients. Why? They’ve been on medications longer. They’ve seen how prices change. They’ve learned that the same pill, bought in bulk, lasts longer and costs less. Employed people trust them more too. Those with jobs are 82% more likely to see generics as safe. Likely because they’re more familiar with cost-saving decisions in other areas of life-like choosing store-brand groceries. But here’s the twist: people with less education often trust their doctors more when they recommend generics. That’s not because they’re less informed-it’s because they rely more on authority figures. Meanwhile, highly educated patients are more likely to research on their own-and sometimes, they find misleading blogs or Reddit threads that amplify fears. And location matters. In the U.S., 94% of patients believe generics are as safe and effective as brand-name drugs. In Greece, that number drops to 70%. Why? Cultural attitudes, media narratives, and even how pharmacists explain substitutions play a role.
How Doctors and Pharmacists Can Build Trust
The single biggest factor in whether a patient accepts a generic? What their doctor says. A 2024 study in PLOS ONE found that when doctors confidently say, “This generic is just as good,” patients are far more likely to agree. In fact, healthcare provider recommendations predicted acceptance with 87.6% accuracy in one machine learning model. So what should doctors say?- “This generic has the same active ingredient as your brand-name drug. The FDA requires it to work the same way.”
- “The only difference is the color or shape. That’s because of the filler ingredients. They don’t change how the medicine works.”
- “I’ve prescribed this generic to hundreds of patients. Their blood tests, symptoms, and side effects are the same as when they took the brand.”
Real Stories: When Generics Work-and When They Don’t
Not every story is perfect. And that’s okay. One Reddit user, u/MedStudent2023, switched their mom from brand-name Synthroid to generic levothyroxine. Her TSH levels stayed stable for two years. They saved $300 a year. Another, u/ChronicPainPatient, had a different experience. Their generic Lyrica caused nausea. The brand never did. So they paid the extra $40 a month. Here’s the truth: those rare cases happen. But they’re not because the generic is inferior. They’re because of differences in inactive ingredients. Some people are sensitive to dyes, preservatives, or binders. That’s why pharmacists are trained to flag substitutions for patients with known allergies or sensitivities. The key? Don’t assume one bad experience means all generics are bad. If a patient has a reaction, switch back-but don’t blame the system. Talk to your provider. Try a different generic manufacturer. There are 10-15 companies making the same drug. One might suit you better.
What’s Changing Now?
The FDA launched a $15 million campaign in January 2024 called “Know Your Options.” It’s targeting myths with clear visuals: side-by-side comparisons of brand and generic pills, lab test results, and patient stories. CVS Health is testing AI tools that analyze your prescription history and send personalized messages: “You’ve taken generic metformin for 3 years. Your A1C hasn’t changed. That’s because it works the same.” Generic manufacturers are now putting QR codes on pill bottles. Scan it, and you’ll see the drug’s FDA approval number, manufacturing site, and bioequivalence data. Kaiser Permanente reduced generic refusal rates by 37% in 2023 using a simple toolkit: pamphlets, videos, and pharmacist-led Q&A sessions during refill pickups.What You Can Do Today
You don’t need to wait for a campaign or a new app. Here’s how to build your own confidence in generics:- Ask your doctor: “Is this generic FDA-approved and bioequivalent?”
- Check the pill: Look up the imprint code (the letters/numbers on the tablet) on Drugs.com or the FDA’s database. You’ll see it matches the brand.
- Track your response: If you switch, note your symptoms, side effects, and lab results for 30-90 days. Most people see no change.
- Ask your pharmacist: “Why does this pill look different?” They’ll explain the inactive ingredients.
- Don’t assume cost = quality. A $2 generic isn’t inferior-it’s efficient.
Generics Aren’t the Future-They’re the Present
In 2023, over 6.8 billion generic prescriptions were filled in the U.S. That’s 90% of all prescriptions. And by 2028, another 227 brand-name drugs will lose patent protection, opening the door to even more generics. The Congressional Budget Office estimates that if patient trust matched reality, Americans could save $1.7 trillion over the next decade. But savings won’t happen unless people believe in the medicine they’re taking. Trust isn’t built by ads. It’s built by conversations. By clear answers. By consistency. By doctors who say, “I believe in this.” The science is settled. The data is clear. The only thing left to change? The story we tell ourselves about what’s in that little pill.Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generic medications to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they deliver the same amount of medicine into your bloodstream at the same rate. Studies show no meaningful difference in effectiveness or safety between generics and brand-name drugs.
Why do generic pills look different from brand-name pills?
The differences in color, shape, or size are due to inactive ingredients like dyes, fillers, or binders. These don’t affect how the drug works. Generic manufacturers use different ingredients to avoid patent issues and reduce costs. The active ingredient-and how your body absorbs it-is identical. If you’re concerned, ask your pharmacist to explain the difference.
Can generics cause different side effects?
Rarely. Side effects come from the active ingredient, which is the same in both brand and generic. But some people are sensitive to inactive ingredients-like certain dyes or preservatives. If you notice new side effects after switching, talk to your doctor. You may need to try a different generic manufacturer, as they use different fillers. This doesn’t mean generics are unsafe-it means your body might react to one filler over another.
Is it safe to switch between different generic brands?
Yes. All FDA-approved generics meet the same strict standards. Switching between different generic manufacturers is common and safe for most people. However, if you have a condition like epilepsy, thyroid disease, or heart failure, your doctor might recommend sticking with one brand to avoid even tiny variations in absorption. Always discuss this with your provider before switching.
Why do insurance companies push generics?
Because generics cost 80-85% less than brand-name drugs. Insurance companies use generics to keep premiums lower for everyone. When you use a generic, your copay is often much lower. It’s not about saving money for the insurer-it’s about making medications affordable for patients. Most insurance plans require you to try generics first before covering a brand-name drug.
How do I know if my generic is FDA-approved?
Look for the imprint code on the pill (the letters or numbers stamped on it). Go to Drugs.com or the FDA’s DailyMed database and enter the code. You’ll see the manufacturer, active ingredient, and FDA approval status. All legally sold generics in the U.S. must be FDA-approved. If you’re unsure, ask your pharmacist to show you the approval details.




Jan Hess
January 16, 2026 AT 00:32