Imagine your doctor prescribes a medication that works perfectly for your condition. You fill the prescription, only to get a call from your pharmacy: step therapy requires you to try three cheaper drugs first. You’re not being stubborn-you’re being blocked by your own insurance plan.
This isn’t a rare glitch. About 40% of all prescription drug plans in the U.S. now use step therapy, also called a "fail-first" policy. It’s a cost-control tactic where insurers force you to try generic or older, cheaper drugs before approving the one your doctor actually prescribed. The idea sounds reasonable: start with what’s affordable. But the reality? For many people, it means months of pain, worsening symptoms, and even permanent damage-all while waiting for paperwork to clear.
How Step Therapy Actually Works
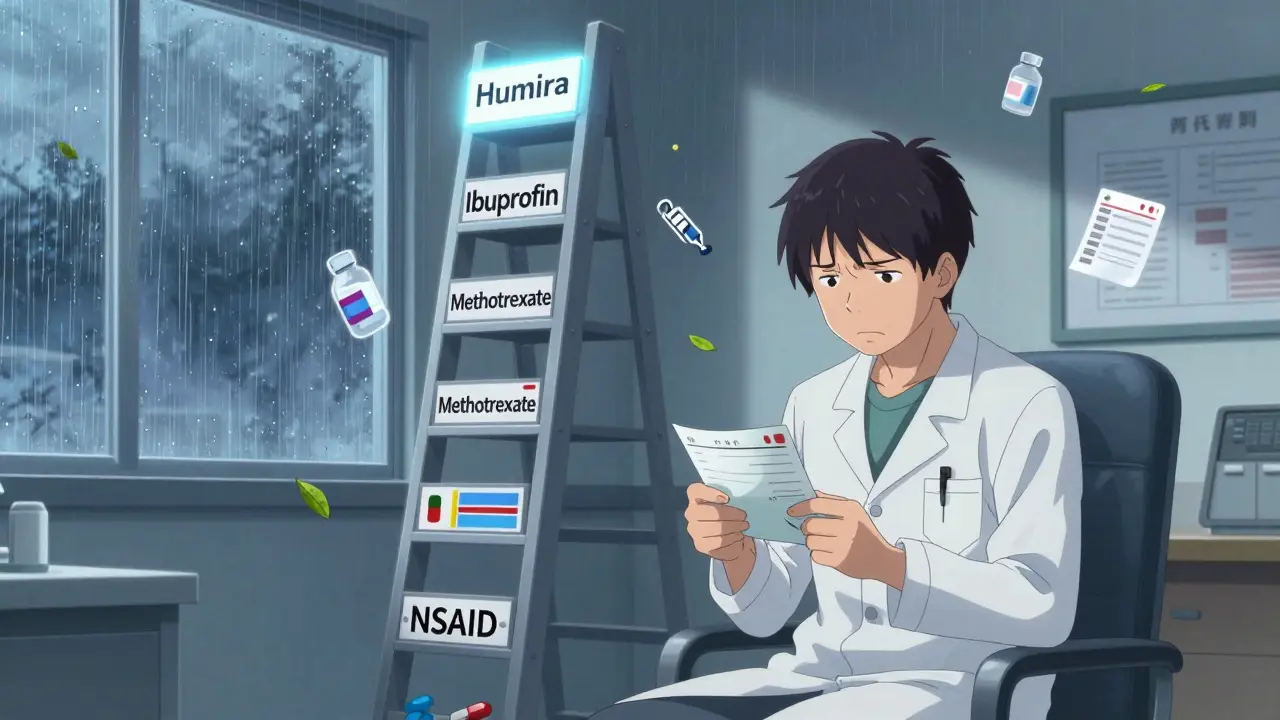
Step therapy isn’t random. Insurers create a ladder of approved drugs for each condition. At the bottom? Generics. At the top? The newer, more expensive brand-name drugs your doctor picked. You must climb each rung before you can reach the top.
For example, if you have rheumatoid arthritis and your doctor prescribes a biologic drug like Humira, your insurer might require you to try at least two NSAIDs (like ibuprofen or naproxen) and one older DMARD (like methotrexate) first. Even if you’ve already tried those drugs and they didn’t work-or made you sick-you still have to go through the motions.
These rules are built into insurance formularies, which are lists of drugs the plan covers. Formularies are designed to save money, not to match your medical history. And here’s the kicker: if you switch jobs or insurance plans, you often have to start the whole ladder over-even if you’ve been on the same medication for years.
Why Insurers Use Step Therapy
Drug prices in the U.S. are among the highest in the world. Brand-name biologics can cost $20,000 to $50,000 a year. Generics? Often under $100. Insurers didn’t create step therapy because they care about your health-they created it because they’re responsible for controlling costs.
According to a 2021 Congressional Budget Office analysis, step therapy can cut pharmaceutical spending by 5% to 15% in some drug categories. That’s millions of dollars saved for insurance companies. But those savings don’t come from lower drug prices-they come from delaying access to the right treatment.
Insurers argue they’re ensuring patients don’t get overprescribed expensive drugs. But the data tells a different story. A 2022 survey by the Arthritis Foundation found that 68% of patients on step therapy experienced negative health outcomes. Nearly half reported their condition got worse while waiting for approval.
When Step Therapy Hurts More Than It Helps
It’s one thing to try a cheaper painkiller before a specialty drug. It’s another when you’re dealing with a chronic, progressive disease.
Take the case of a Reddit user named "ChronicPainWarrior," who had to fail three different NSAIDs over six months before getting approval for a biologic for rheumatoid arthritis. By the time the insurance approved it, their joints were permanently damaged. That’s not an outlier-it’s the norm.
Conditions like multiple sclerosis, Crohn’s disease, lupus, and severe psoriasis don’t wait. Every week of delay can mean irreversible nerve damage, organ scarring, or loss of mobility. The American College of Rheumatology says step therapy puts patients at risk of disease progression, and they’ve publicly opposed it.
Even worse, the appeals process takes weeks. Blue Cross Blue Shield of Michigan says it takes 72 business hours for a standard request. But that’s just their internal timeline. Real-world reports from patients show it often takes four to eight weeks. And if your doctor’s office has to resubmit paperwork because of a missing form? That adds another two weeks.
Doctors are drowning in paperwork. On average, they spend 18.3 hours a week just handling prior authorizations and step therapy requests. That’s nearly half a workday-time that could be spent treating patients, not fighting insurers.

What You Can Do: Step Therapy Exceptions
You’re not powerless. Federal and state laws require insurers to allow exceptions. The Safe Step Act (still pending at the federal level) outlines five clear situations where insurers must bypass step therapy:
- The required drug was already tried and failed
- Delaying treatment could cause severe or irreversible harm
- The required drug is contraindicated for you
- The required drug would prevent you from doing daily activities
- You’re already stable on your current drug
If your doctor says you meet any of these, they can file a step therapy exception. But here’s the catch: you need documentation. Not just a note. You need medical records showing:
- Previous prescriptions you tried
- Side effects you experienced
- Lab results showing disease progression
- Letters from your specialist explaining why the alternative won’t work
Some insurers have online portals for exceptions. Others still require faxed forms. The process is inconsistent, slow, and frustrating. But it’s your only path to getting the right treatment.
State Laws Vary-And That Matters
As of 2026, 29 states have passed laws to protect patients from abusive step therapy practices. But here’s the loophole: these laws only apply to fully-insured plans. That means if your employer self-insures (and 61% of Americans do), state laws don’t touch your coverage.
Self-insured plans are regulated by the federal government under ERISA. And right now, there’s no federal rule forcing them to provide fast, fair exceptions. That’s why the Safe Step Act keeps getting reintroduced-it’s meant to close that gap.
Even within states that have protections, rules differ. Some require insurers to respond within 24 hours for urgent cases. Others allow up to 72 hours. A few even require written explanations for denials. But if your plan is self-insured? You’re at the mercy of the insurer’s internal policies.

Generics Aren’t Always the Answer
It’s easy to assume generics are just as good. And for many conditions, they are. But for complex diseases, generics don’t exist. Biologics, for example, are made from living cells. You can’t copy them like you can with a pill. The closest thing is a "biosimilar," which is similar-but not identical.
Even when generics exist, they might not work for you. A 2023 GoodRx survey found that 17% of patients actually did well on the required generic. But 73% of patients who needed step therapy exceptions took 1 to 3 months to get approval. And 28% gave up entirely-either because the process was too long, too confusing, or too expensive to keep fighting.
Insurers know this. That’s why they’ve started partnering with pharmaceutical companies on co-pay cards and patient assistance programs. If you can get a free or discounted version of the brand-name drug through the manufacturer, sometimes you can skip the step therapy hurdle entirely. But these programs are hard to find, often require income verification, and don’t cover all drugs.
What’s Next? The Future of Step Therapy
Step therapy isn’t going away. Insurers are using it more, not less. Avalere Health predicts it will cover 55% of specialty drug prescriptions by 2025. That’s up from 40% today.
But patient advocacy groups are pushing back. The Partnership to Fight Chronic Disease is demanding insurers cut exception processing times from four weeks to under seven days. Some states are starting to require real-time online approvals. Others are forcing insurers to publish their step therapy rules in plain language.
The real solution? A federal standard. One that applies to all plans-fully insured or self-insured. One that forces insurers to respond within days, not weeks. One that recognizes that when a doctor says a drug is necessary, it shouldn’t take a legal battle to get it.
Until then, your best defense is knowledge. Know your plan’s formulary. Know your rights. And don’t let your doctor’s prescription sit on a desk for months while you wait for a bureaucrat to sign off.
What to Do Right Now
If you’re facing step therapy:
- Ask your doctor if they’ve filed an exception. Many don’t unless you ask.
- Request a copy of your plan’s step therapy policy. It’s required by law to be available.
- Document everything: dates, names, prescriptions tried, side effects, lab results.
- If you’re denied, appeal immediately. Most plans allow one appeal, but you can escalate to your state’s insurance commissioner if needed.
- Check if the drug manufacturer offers patient assistance. Many do-especially for expensive biologics.
Step therapy was meant to save money. But when it costs you your health, it’s not saving anything-it’s stealing time, mobility, and peace of mind.






Clay .Haeber
January 13, 2026 AT 02:27