How to Buy Cheap Generic Tetracycline Online Safely
August 19 2025EU GMP Annex 1: What It Means for Pharmaceutical Quality and Safety
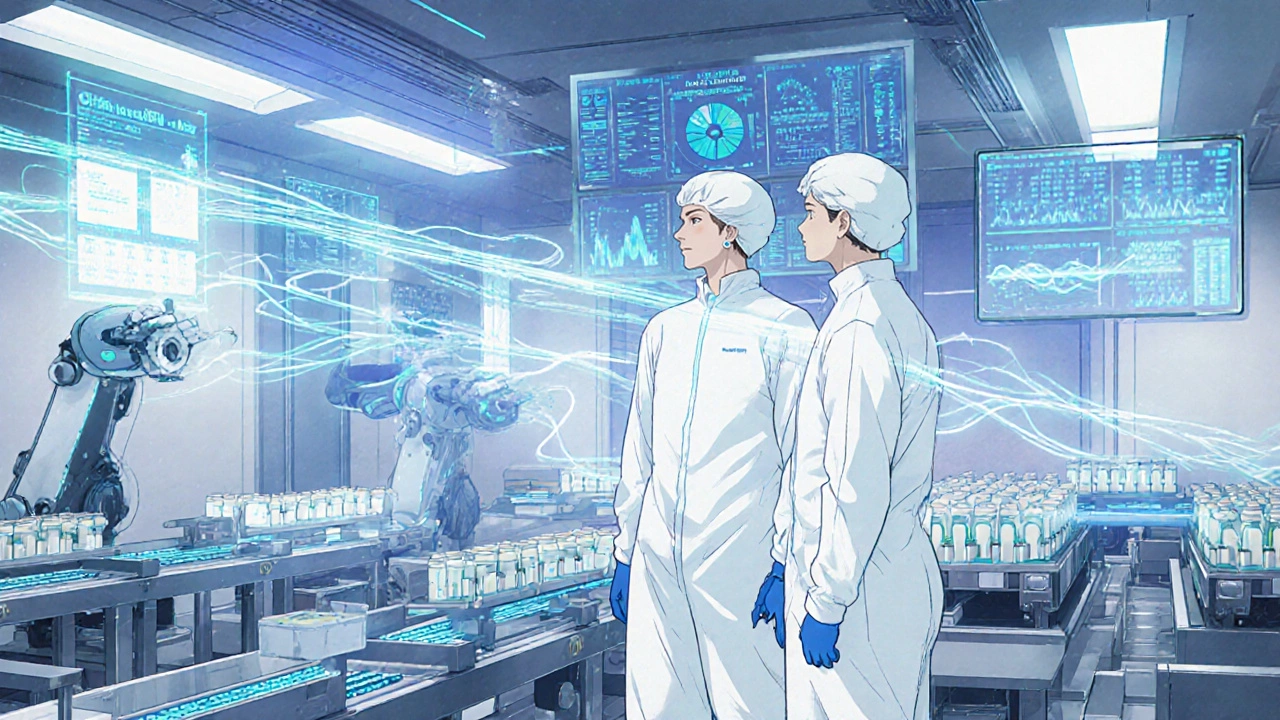
When it comes to making medicines that are safe to inject, inhale, or infuse into the body, EU GMP Annex 1, the European Union’s strictest set of rules for sterile pharmaceutical manufacturing. It’s not just a guideline—it’s the law for anyone producing injectables, eye drops, or IV solutions in Europe or exporting to Europe. This document doesn’t just talk about cleanliness. It demands proof—real-time monitoring, validated processes, and zero tolerance for contamination. If your drug is meant to go directly into the bloodstream, Annex 1 is the barrier between life and death.
It’s not just about clean rooms. sterile manufacturing, the process of making medicines without any living microbes under Annex 1 requires controlled airflow, automated equipment, and staff trained to move like ghosts—no unnecessary motion, no skin flakes, no breath near the product. Even the way you wear gloves matters. The rules cover everything from how air is filtered to how often surfaces are swabbed for bacteria. And it’s not just for big labs. Small contract manufacturers, compounding pharmacies, and even hospitals making IV bags must follow these standards if they want their products to be sold in the EU.
What makes Annex 1 different from older rules? It’s science-driven. It doesn’t say "just clean it." It says: "prove the cleaning works," "show the air won’t carry contamination," and "monitor every batch in real time." It forces manufacturers to think like a microbe—where would it hide? How would it spread? That’s why you’ll see posts here about temperature and humidity control for medication storage, or why dissolution profiles matter for generics. Those aren’t random topics. They’re all pieces of the same puzzle: ensuring every pill, every injection, every drop is exactly what it claims to be. GMP compliance, the system of practices that guarantee medicine quality isn’t about paperwork. It’s about preventing a child from getting a contaminated IV bag or a senior getting a false dose because a vial was mishandled.
And it’s evolving. The latest version, updated in 2022, didn’t just tweak old rules—it rewrote the playbook for contamination control. It demands more data, more automation, and more accountability. That’s why posts on this page cover everything from how to store meds properly to why bioequivalence matters for critical drugs. Because if a drug isn’t made right, it doesn’t matter how well it works on paper. You can’t trust it in the body. That’s the core of Annex 1: trust built on proof, not promises.
Below, you’ll find practical guides from real-world scenarios—how to spot degradation in stored meds, why timing matters for blood pressure drugs, how to use naloxone in an emergency, and what happens when a generic doesn’t match the brand. These aren’t just tips. They’re all connected to the same mission: making sure the medicine you take does what it’s supposed to—without putting you at risk.
 29 Nov
29 Nov
Current GMP Standards: Detailed Requirements Explained for 2025
Current GMP standards in 2025 require modern technology, digital data integrity, and strict supply chain controls. Learn the nine core requirements, key differences between FDA and EU rules, and how to stay compliant.
Read More...