Antihistamine Safety Checker
Check Your Medication for Dangerous Antihistamines
Elderly patients should avoid first-generation antihistamines like diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine. These can cause confusion, falls, and increase dementia risk. This tool checks if your medication contains dangerous ingredients.
Potential Danger
This medication contains first-generation antihistamines which may be unsafe for elderly patients.
Recommended action: Consult your doctor about safer alternatives like loratadine (Claritin), cetirizine (Zyrtec), or fexofenadine (Allegra).
Every year, millions of older adults reach for over-the-counter sleep aids or allergy pills without realizing they’re putting themselves at serious risk. Medications like Benadryl and Unisom may seem harmless-cheap, easy to find, and marketed as gentle solutions for trouble sleeping or a runny nose. But for people over 65, these drugs can trigger confusion, falls, memory loss, and even accelerate dementia. The science is clear: first-generation antihistamines are unsafe for elderly patients, and continuing to use them is like playing Russian roulette with brain health.
Why Older Adults React Differently to Antihistamines
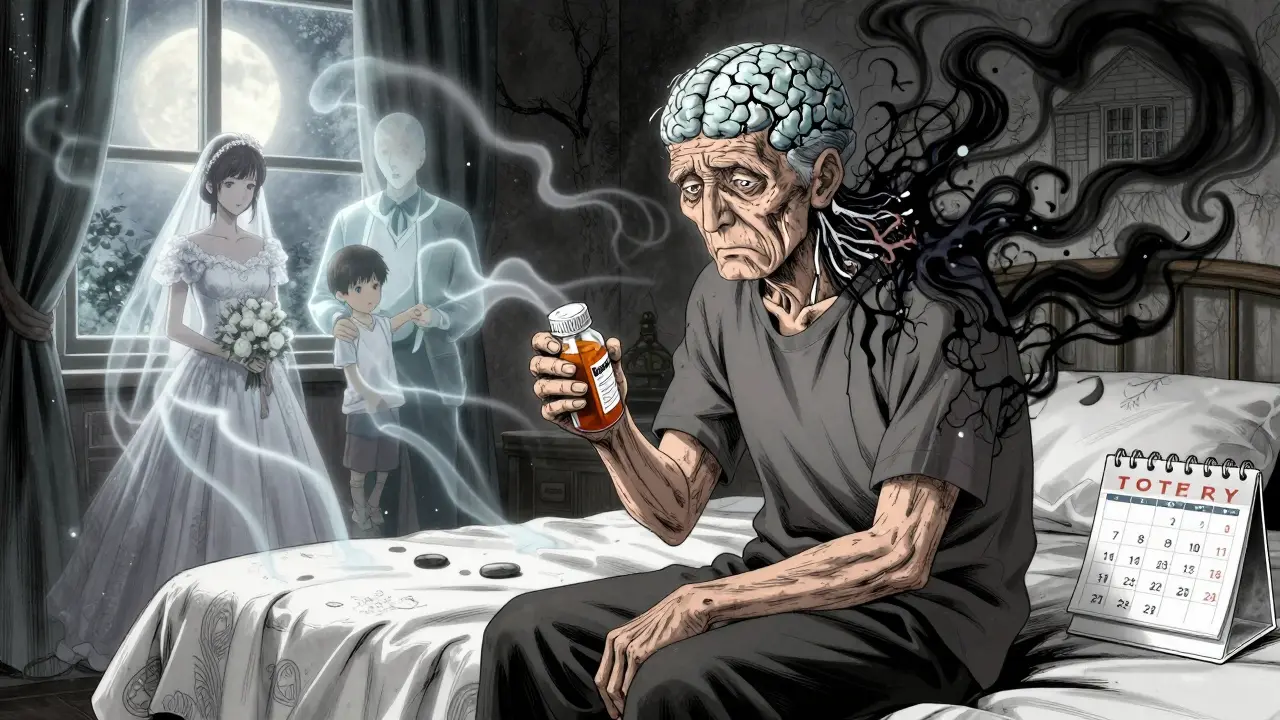
As we age, our bodies change in ways that make drugs behave differently. The liver and kidneys don’t process medications as efficiently. Blood flow to the brain slows. And the brain itself produces less acetylcholine-a key chemical for memory, focus, and muscle control. First-generation antihistamines like diphenhydramine and doxylamine don’t just block histamine; they also block acetylcholine receptors. That’s called an anticholinergic effect. In younger people, the brain can compensate. In older adults, it can’t. This double hit-reducing acetylcholine while also blocking its receptors-is why even a single dose of Benadryl can leave an elderly person feeling foggy, dizzy, or disoriented. One study found that elderly patients taking these drugs were over twice as likely to suffer a serious fall or fracture. And it’s not just falls. These medications can cause urinary retention, constipation, blurred vision, dry mouth, and even acute delirium. Some patients wake up thinking they’re in a different house, or try to pack their bags to ‘go home’-even when they’ve lived in the same place for 40 years.The Two Types of Antihistamines: A Clear Divide
Not all antihistamines are created equal. There are two major types, and the difference matters more than most people realize. First-generation antihistamines include diphenhydramine (Benadryl), chlorpheniramine, hydroxyzine, and doxylamine (Unisom SleepTabs). They’re lipophilic-meaning they easily slip through the blood-brain barrier. That’s why they make you sleepy. But that same property makes them dangerous for older adults. These drugs are the ones found in many nighttime pain relievers, cold medicines, and sleep aids. They’re cheap, widely available, and often recommended by well-meaning family members who don’t know the risks. Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) were designed differently. They’re polar molecules that stay mostly outside the brain. They relieve allergies just as well, but they don’t cause the same level of drowsiness or cognitive side effects. Studies show they don’t increase the risk of falls, confusion, or dementia. In fact, they’re now the standard of care for older adults who need allergy or sleep help.The Dementia Connection
It’s not just about confusion after taking a pill. Long-term use of first-generation antihistamines is linked to a real, measurable rise in dementia risk. A landmark 2015 study in JAMA Internal Medicine followed 3,434 adults over age 65 for an average of seven years. Those who took the equivalent of three or more years of daily anticholinergic medication-including diphenhydramine-had a 54% higher chance of developing dementia than those who used these drugs for less than three months. The effect wasn’t small. It wasn’t theoretical. It was statistically significant, even after adjusting for other health factors. And the risk climbed with longer use. This isn’t just about memory lapses. It’s about irreversible brain changes. The same drugs that help you fall asleep tonight might be quietly eroding your ability to recognize your own children tomorrow.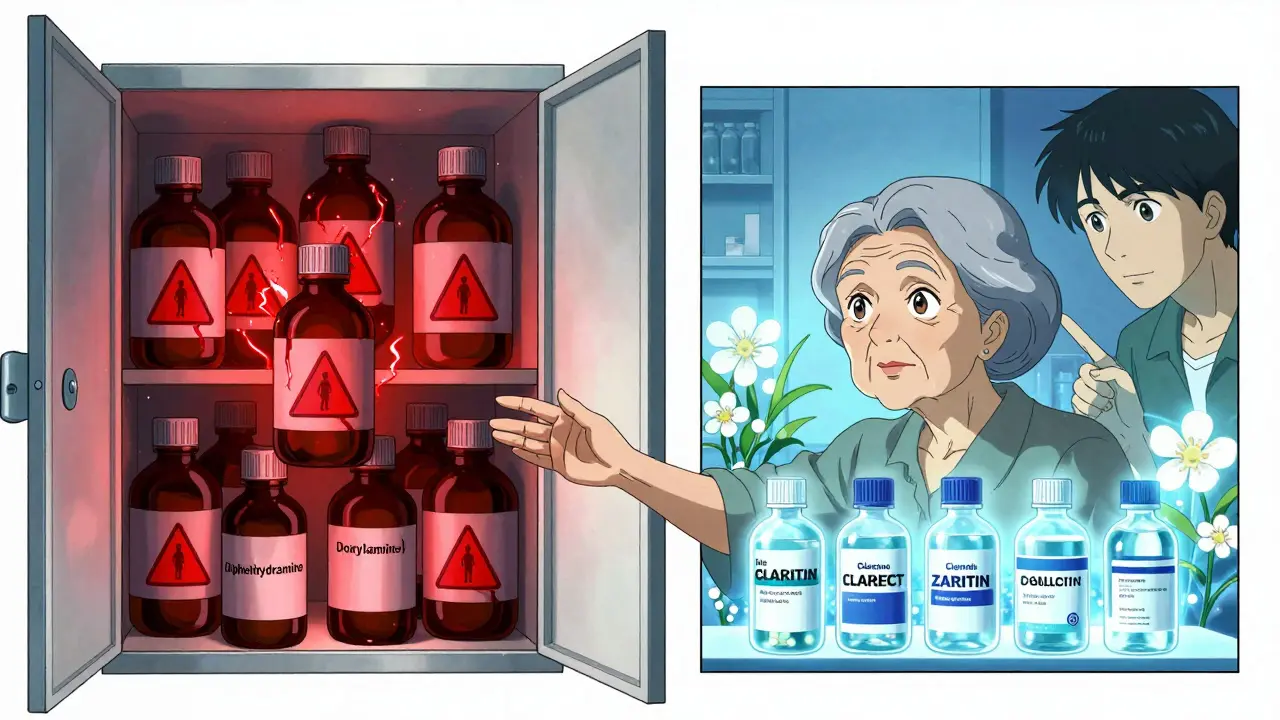
What’s Really in Your Medicine Cabinet?
Here’s the problem: most people don’t realize they’re taking a first-generation antihistamine. You might think you’re just taking a sleep aid, a cold tablet, or a pain reliever. But look at the ingredient list. If you see diphenhydramine, doxylamine, or chlorpheniramine, you’re on a high-risk drug. Common products hiding these ingredients:- Benadryl (diphenhydramine)
- Unisom SleepTabs (doxylamine)
- NyQuil, Tylenol PM, Advil PM (diphenhydramine)
- Excedrin PM (diphenhydramine)
- Dimetapp Cold & Allergy (brompheniramine)
- Many generic store-brand sleep aids
What Should Elderly Patients Use Instead?
The good news? There are safe, effective alternatives.- Loratadine (Claritin) - 10 mg once daily. Non-sedating. Safe for kidneys and liver.
- Cetirizine (Zyrtec) - 5 mg once daily. Slightly more sedating than loratadine, but still far safer than Benadryl. Ideal for moderate allergies.
- Fexofenadine (Allegra) - 60 mg twice daily. Least likely to cause drowsiness. Good for people with kidney issues.
- Improving sleep hygiene (dark room, no screens before bed, consistent schedule)
- Using melatonin (low dose, 0.5-1 mg) under medical supervision
- Trying cognitive behavioral therapy for insomnia (CBT-I), which is proven more effective than pills for long-term sleep
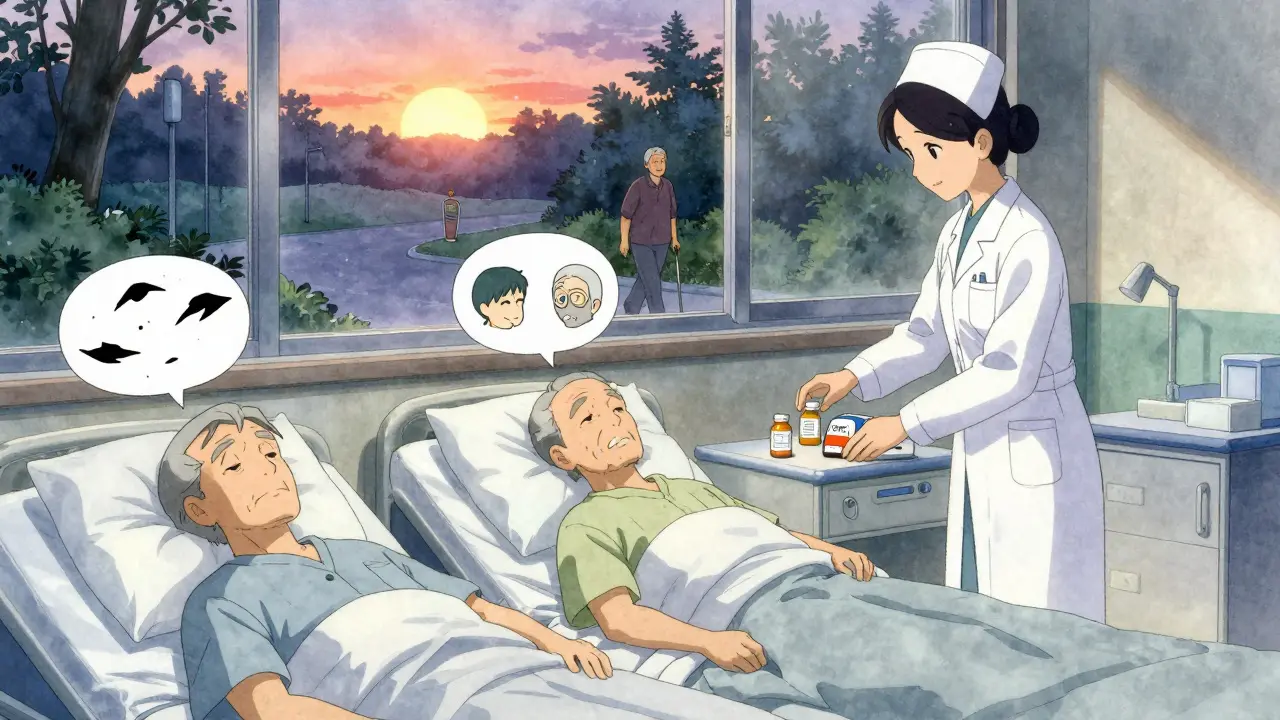
What Doctors and Families Need to Do
Healthcare providers must stop prescribing or recommending first-generation antihistamines to older patients. The American Geriatrics Society’s Beers Criteria has listed them as potentially inappropriate since 1991-and updated the warning in 2019 to call them ‘high-risk.’ Yet they’re still sold on every pharmacy shelf. Families need to take action too. If you’re helping care for an older relative:- Check every pill bottle, especially nighttime medicines.
- Ask the doctor: ‘Is this antihistamine first-generation?’
- Replace Benadryl with Claritin or Zyrtec.
- Remove all PM pain relievers from the medicine cabinet.
- Use saline nasal sprays, HEPA filters, and allergen-proof bedding to reduce allergy triggers without drugs.
The Bigger Picture: A Preventable Epidemic
We’re talking about a public health failure. First-generation antihistamines are cheap, widely available, and heavily marketed. The FDA hasn’t required stronger warnings on labels, despite years of evidence. Sales of diphenhydramine alone exceed $350 million a year in the U.S.-mostly bought by people over 65. But here’s the hopeful part: we can fix this. A 2023 study showed that when geriatric clinics actively educate patients and families about anticholinergic risks, use of these drugs drops by 12% in just two years. That’s 12% fewer falls, 12% fewer hospital visits, 12% fewer cases of avoidable dementia. Experts estimate that eliminating first-generation antihistamines in older adults could prevent 250,000 falls and 50,000 dementia cases every year in the U.S. alone. That’s not just numbers. That’s mothers remembering their grandchildren. That’s fathers walking to the park without help. That’s independence preserved.Bottom Line: Stop the Harm
If you’re over 65 and taking Benadryl, Unisom, or any nighttime medicine for sleep or allergies, stop. Don’t wait for a doctor to tell you. Don’t assume it’s safe because it’s over-the-counter. The science is overwhelming: these drugs are dangerous for older adults. Switch to loratadine, cetirizine, or fexofenadine. Talk to your pharmacist. Ask your doctor to review your entire medication list. Remove all PM pain relievers from your home. This isn’t about being overly cautious. It’s about protecting the most vulnerable part of your brain-the part that holds your memories, your identity, your sense of self. You don’t need a sleeping pill that steals your mind. You need a solution that lets you rest without risking your future.Are all antihistamines dangerous for elderly people?
No. Only first-generation antihistamines like diphenhydramine (Benadryl) and doxylamine (Unisom) are dangerous for older adults. These drugs cross into the brain and block acetylcholine, leading to confusion, falls, and increased dementia risk. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are safe for elderly patients because they don’t enter the brain in significant amounts and cause minimal side effects.
Can I take Benadryl occasionally for sleep if I’m over 65?
Even occasional use is risky. A single dose of diphenhydramine can cause next-day drowsiness, dizziness, and impaired balance-increasing the chance of a fall. In older adults, even one fall can lead to a hip fracture, hospitalization, or permanent loss of independence. There’s no safe ‘occasional’ dose when it comes to first-generation antihistamines. Safer alternatives exist, so avoid Benadryl entirely.
What should I do if my parent is already taking Benadryl daily?
Don’t stop abruptly without talking to a doctor, especially if it’s been used long-term. But do schedule a medication review. Ask the doctor to replace it with a second-generation antihistamine like Claritin or Zyrtec for allergies, or consider non-drug options like melatonin or CBT-I for sleep. Check all medicine bottles for hidden diphenhydramine in cold or pain meds. Remove all PM formulations from the home.
Do second-generation antihistamines work as well as Benadryl?
Yes, for allergies. Studies show cetirizine and loratadine are just as effective as diphenhydramine for treating hay fever, hives, and itchy skin. The only difference is safety. Second-generation options don’t cause drowsiness or cognitive side effects. For sleep, they don’t work as sedatives-because they’re not designed to. That’s actually a good thing. Better sleep comes from habits, not brain-slowing drugs.
Why haven’t these drugs been taken off the market?
Because they’re not prescription drugs-they’re over-the-counter. The FDA doesn’t remove OTC products unless they’re proven unsafe for *everyone*, not just high-risk groups. Even though the American Geriatrics Society has warned against them since 1991, manufacturers aren’t required to pull them. Some companies added warning labels in 2020, but the drugs remain widely available. The burden is on patients and caregivers to recognize the risk and choose safer options.
Can antihistamines cause permanent brain damage?
Long-term use of first-generation antihistamines is linked to an increased risk of dementia, suggesting they may contribute to lasting cognitive decline. While stopping the drug can reverse acute confusion and delirium, the structural brain changes associated with prolonged anticholinergic exposure may not be fully reversible. The best strategy is prevention: avoid these drugs entirely in older adults to protect long-term brain health.



Napoleon Huere
January 26, 2026 AT 01:21