What Is Triple Inhaler Therapy for COPD?
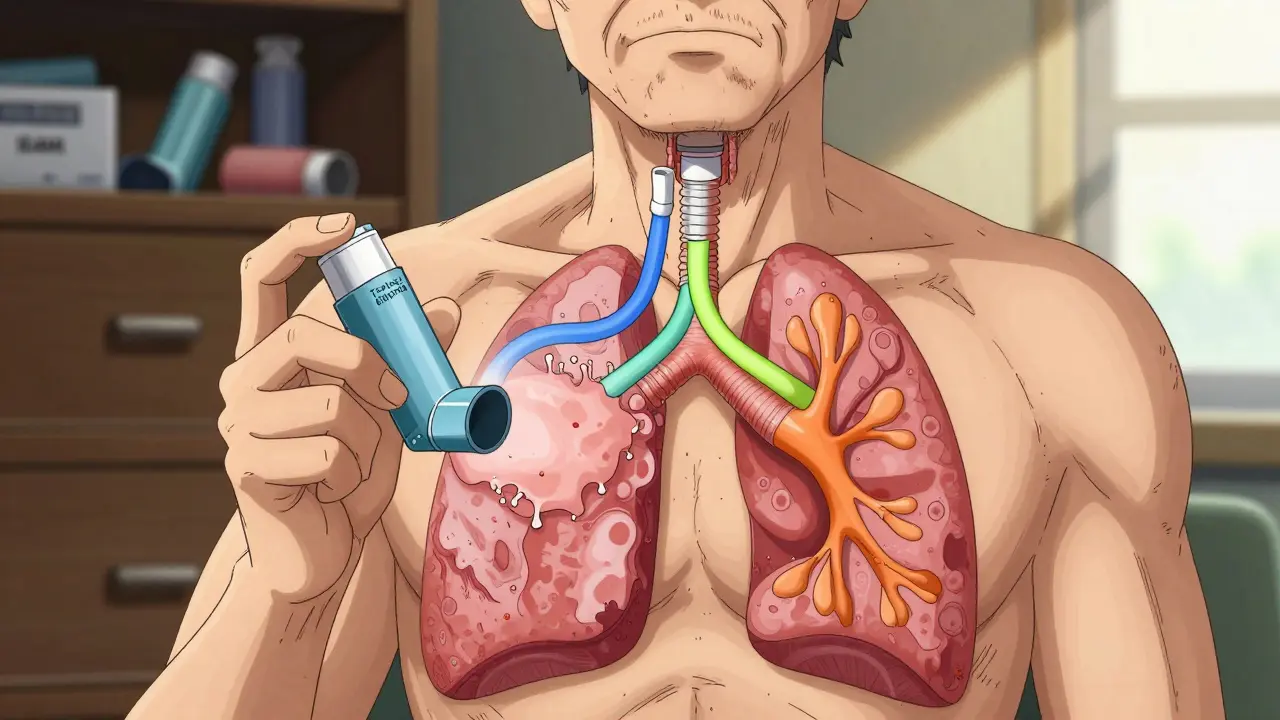
Chronic Obstructive Pulmonary Disease (COPD) isn’t just about feeling out of breath. For many, it’s a cycle of worsening symptoms, hospital visits, and lost days at work or with family. Triple inhaler therapy combines three medications-an inhaled corticosteroid (ICS), a long-acting muscarinic antagonist (LAMA), and a long-acting beta-agonist (LABA)-into one treatment plan. The goal? Stop flare-ups before they start.
This isn’t new. But in 2023, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) updated its guidelines to make it clearer: triple therapy isn’t for everyone. It’s for a specific group-people with moderate to severe COPD who’ve had two or more moderate flare-ups, or one severe one, in the past year. And even then, it only works well if their blood eosinophil count is 300 cells/µL or higher.
Think of it like fixing a leaky roof. One patch (a bronchodilator) might help for a while. But if the roof is rotting (inflammation) and the gutters are clogged (mucus), you need more than one fix. ICS reduces swelling, LAMA opens airways by blocking tight muscles, and LABA keeps them open longer. Together, they tackle all three problems at once.
Single vs. Multiple Inhalers: Why One Device Matters
There are two ways to take triple therapy. One is using three separate inhalers. The other is using a single device that holds all three medicines. Sounds simple, right? But the difference isn’t just convenience-it’s survival.
Real-world data from the TARGET study shows people using a single inhaler (SITT) stick to their treatment 15-20% better than those juggling two or three devices. Why? Because forgetting one inhaler means skipping a whole class of medicine. One study found 43% of patients on multiple inhalers forgot doses. Another 29% got confused about which one to use when.
Switching from multiple inhalers to a single one didn’t just improve adherence-it cut exacerbations by 37% in the six months after the switch. Patients said it was simpler. Less to carry. Less to remember. One woman in Brisbane told her doctor, “I used to have a whole drawer full of inhalers. Now I just grab one. I actually take it every day.”
The most common single-inhaler devices are:
- Trelegy Ellipta (fluticasone furoate/umeclidinium/vilanterol): Once daily, 100/62.5/25 mcg
- Trimbow (budesonide/glycopyrronium/formoterol): Twice daily, 320/18/9 mcg
- QBreva (beclomethasone/glycopyrronium/formoterol): Twice daily
Extrafine particle versions like Trimbow reach deeper into the lungs, which may improve effectiveness. But the biggest factor isn’t the brand-it’s whether you use it every day.
Who Benefits Most-and Who Should Avoid It
Not everyone with COPD needs triple therapy. In fact, most don’t.
Studies like IMPACT and ETHOS showed that triple therapy reduces moderate-to-severe exacerbations by about 25% compared to dual bronchodilator therapy-but only in people with high eosinophils. Blood eosinophils are a marker of inflammation. If your count is below 100 cells/µL, triple therapy offers little to no benefit. If it’s above 300, the reduction in flare-ups can be life-changing.
But here’s the catch: some of the benefit seen in trials might be misleading. Dr. John Blakey from the University of Western Australia points out that in many trials, patients were taken off their ICS before switching to dual therapy. That’s like turning off a fire alarm before testing if the sprinklers work. When real-world data from the UK tracked 31,000 patients without abrupt ICS withdrawal, the difference between triple and dual therapy vanished.
And there’s a serious risk: pneumonia. Fluticasone-based inhalers (like Trelegy) increase pneumonia risk by 83% compared to budesonide-based ones (like Trimbow). The FDA requires a black box warning for this. If you’re over 65, smoke, or have had pneumonia before, this isn’t just a side effect-it’s a red flag.
Bottom line: Triple therapy is only for patients who meet all three criteria:
- Have had ≥2 moderate or ≥1 severe exacerbation in the past year
- Have blood eosinophil count ≥300 cells/µL
- Are still having flare-ups despite using LAMA/LABA alone
If you don’t meet all three, you’re not helping yourself-you’re risking harm.

The Cost Problem: When Medicine Becomes Unaffordable
Triple inhalers are expensive. In the U.S., brand-name versions like Trelegy Ellipta can cost $75-$150 per month out-of-pocket. For Medicare beneficiaries on fixed incomes, that’s a choice between medicine and groceries.
A 2022 study found 22.3% of patients skipped doses because of cost. That’s not noncompliance-it’s survival math. One man in Ohio told his pulmonologist, “I take half my dose every other day. It’s not ideal, but I can’t afford the full prescription.”
Even in Australia, where the PBS subsidizes many COPD drugs, triple therapy isn’t always covered unless you meet strict criteria. Some patients end up paying hundreds a year just to keep their inhaler.
There are solutions: medication synchronization programs, generic alternatives (when available), and patient assistance programs from manufacturers. But the system isn’t designed for this. Doctors need to ask about cost-not just adherence. A simple question like, “Can you afford this?” can prevent hospital readmissions.
Technique Matters More Than You Think
Even if you have the right medicine, the wrong technique makes it useless. Studies show 50-70% of patients who seem to “not respond” to triple therapy are just using their inhaler wrong.
Ellipta devices require a specific breath pattern: inhale deeply and hold for 5 seconds. Metered-dose inhalers need precise timing between pressing the canister and breathing in. Mistakes mean less than 20% of the dose reaches the lungs.
One study found it takes 7.2 minutes to teach proper Ellipta use-almost twice as long as a standard metered-dose inhaler. Yet many clinics rush through it. Nurses don’t have time. Doctors assume patients “know how.”
Ask your doctor for a technique check every time you refill. Use a checklist. Film yourself using the inhaler and compare it to a video from the manufacturer. If you’re still wheezing after three months, it’s not the drug-it’s the delivery.

What’s Next for COPD Treatment?
The future of COPD isn’t just more inhalers. It’s smarter inhalers.
Researchers are now testing whether fractional exhaled nitric oxide (FeNO) can predict who responds to ICS better than eosinophils. Early results from the EXACT study suggest it might. If true, we could move from a one-size-fits-all biomarker to a more precise, personalized approach.
Also on the horizon: biologics like dupilumab, originally developed for asthma and eczema. The LIBERTY POSEIDON trial shows it reduces exacerbations in COPD patients with high eosinophils-potentially offering an alternative to steroids.
But for now, triple inhaler therapy remains the most effective tool we have for a specific group of patients. It’s not magic. It’s medicine-carefully targeted, carefully monitored, and carefully used.
When to Talk to Your Doctor
If you’ve had two or more COPD flare-ups in the last year, ask your doctor:
- “What’s my blood eosinophil count?”
- “Have I been using my inhaler correctly?”
- “Is triple therapy right for me-or am I just taking extra pills?”
- “Can we try a cheaper option or a generic?”
Don’t assume more medicine equals better results. Sometimes, less is more. And sometimes, the right medicine, used correctly, can keep you out of the hospital-and home with your family.




Saylor Frye
January 6, 2026 AT 10:48