Drinking a glass of grapefruit juice in the morning might seem like a healthy habit-until it starts messing with your meds. This isn’t just a myth or a vague warning on a label. Grapefruit juice can turn your prescribed medication into something dangerous, even deadly. And it doesn’t matter if you drink it an hour before or after your pill. The damage is already done.
Why Grapefruit Juice Is So Dangerous With Medications
It all comes down to one enzyme in your gut: CYP3A4. This enzyme is like a bouncer at a club-it decides which drugs get into your bloodstream and how much. Normally, it breaks down about half of the oral medications you take before they even reach your blood. Grapefruit juice doesn’t just slow down this bouncer. It knocks it out cold. The furanocoumarins in grapefruit-mainly bergamottin and 6',7'-dihydroxybergamottin-stick to CYP3A4 and permanently disable it. Your body can’t make new enzymes fast enough. It takes 24 to 72 hours to recover. That means one glass of juice can affect your meds for days.And here’s the kicker: you can’t tell who’s at risk. Some people’s guts have more CYP3A4 than others. One study found that after drinking grapefruit juice, some people had 8 times more drug in their blood than others. No test can predict who’s more sensitive. So if your drug is on the list, the safest move is to avoid grapefruit entirely.
Which Medications Are Most at Risk?
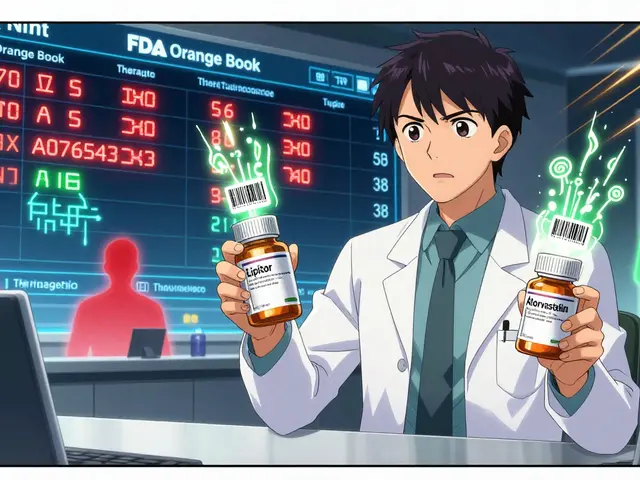
More than 85 prescription drugs in North America interact with grapefruit juice. Of those, 43 can cause life-threatening reactions. Here are the big ones:- Statins (cholesterol drugs): Simvastatin (Zocor) is the worst offender. Just one glass a day for three days can triple your blood levels. That raises your risk of rhabdomyolysis-a condition where muscle tissue breaks down and can cause kidney failure. Atorvastatin (Lipitor) is less risky, but still dangerous. Pravastatin and rosuvastatin? Safe. No interaction.
- Calcium channel blockers (blood pressure meds): Felodipine (Plendil) sees a 5-fold increase in blood levels. Nifedipine (Procardia) jumps 3.3 times. Amlodipine (Norvasc)? No problem. The difference comes down to how much each drug relies on CYP3A4 to break down.
- Immunosuppressants: Cyclosporine (Neoral), used after organ transplants, can spike 50-60% in concentration. That means higher risk of kidney damage. Tacrolimus is a safer alternative.
- Antiarrhythmics: Amiodarone (Cordarone) can increase plasma levels by 30-40%, raising the chance of dangerous heart rhythms.
- Others: Some anxiety meds, sedatives, and even certain cancer drugs like docetaxel are affected. But drugs like trazodone and zolpidem? Minimal to no interaction.
Not all drugs react the same way. Some are barely touched. Others? One sip can push you over the edge.
What About Other Citrus Fruits?
Not all citrus is created equal. Seville oranges-used in bitter marmalade-and pomelos contain the same furanocoumarins as grapefruit. So if you’re on a risky medication, skip those too. Sweet oranges (like navel or Valencia), lemons, and limes? Safe. They don’t have the compounds that wreck CYP3A4. The European Medicines Agency confirmed this in 2022. So you can still have your orange juice with breakfast. Just leave the grapefruit out.
It’s Not Just Juice-It’s Everything
People think it’s only about juice. But it’s not. Whole grapefruit? Same risk. Grapefruit extract in supplements? Even worse-concentrated. Even grapefruit-flavored sodas or candies can contain enough furanocoumarins to cause trouble. And pasteurized juice? Doesn’t matter. The harmful compounds survive heat treatment. Fresh-squeezed might be stronger, but store-bought isn’t safe either. The FDA says it doesn’t matter how you get it. If it’s grapefruit, avoid it.Why This Isn’t Just a ‘Be Careful’ Warning
This isn’t a ‘maybe’ situation. It’s a medical fact backed by decades of research. In 1989, Canadian researchers discovered this by accident. They were testing felodipine and noticed patients had way higher drug levels than expected. Turns out, they’d been drinking grapefruit juice. Since then, over 100 clinical studies have confirmed it. The FDA started requiring drug labels to warn about grapefruit in 2014. In 2020, they updated their guidelines to make testing for this interaction mandatory during drug development.And it’s not just a lab thing. Real people are getting hurt. A 2014 study showed the risk of rhabdomyolysis from simvastatin and grapefruit jumped from 0.04 to 0.44 cases per 100 person-years. That’s a tenfold increase. For older adults-who often take 3 to 5 medications and are more likely to drink grapefruit juice-it’s even riskier. One in four grapefruit consumers in the U.S. is over 65.
What Should You Do?
Step 1: Look at your meds. If you’re on statins, blood pressure pills, immunosuppressants, or antiarrhythmics, assume grapefruit is off-limits until you check. Step 2: Talk to your pharmacist. They’re trained to catch this stuff. A 2021 study found 89% of community pharmacists screen for grapefruit interactions when dispensing meds. Ask them: “Does this interact with grapefruit?” Don’t assume they’ll tell you unless you ask. Step 3: Keep a list. Write down every pill, supplement, and OTC drug you take. Bring it to every appointment. Many patients don’t even realize their allergy meds or sleep aids could be risky. Step 4: If your drug is risky, ask for an alternative. Switching from simvastatin to pravastatin or rosuvastatin is safe and common. Switching from cyclosporine to tacrolimus is an option for transplant patients. Your doctor can find a drug that works without the danger.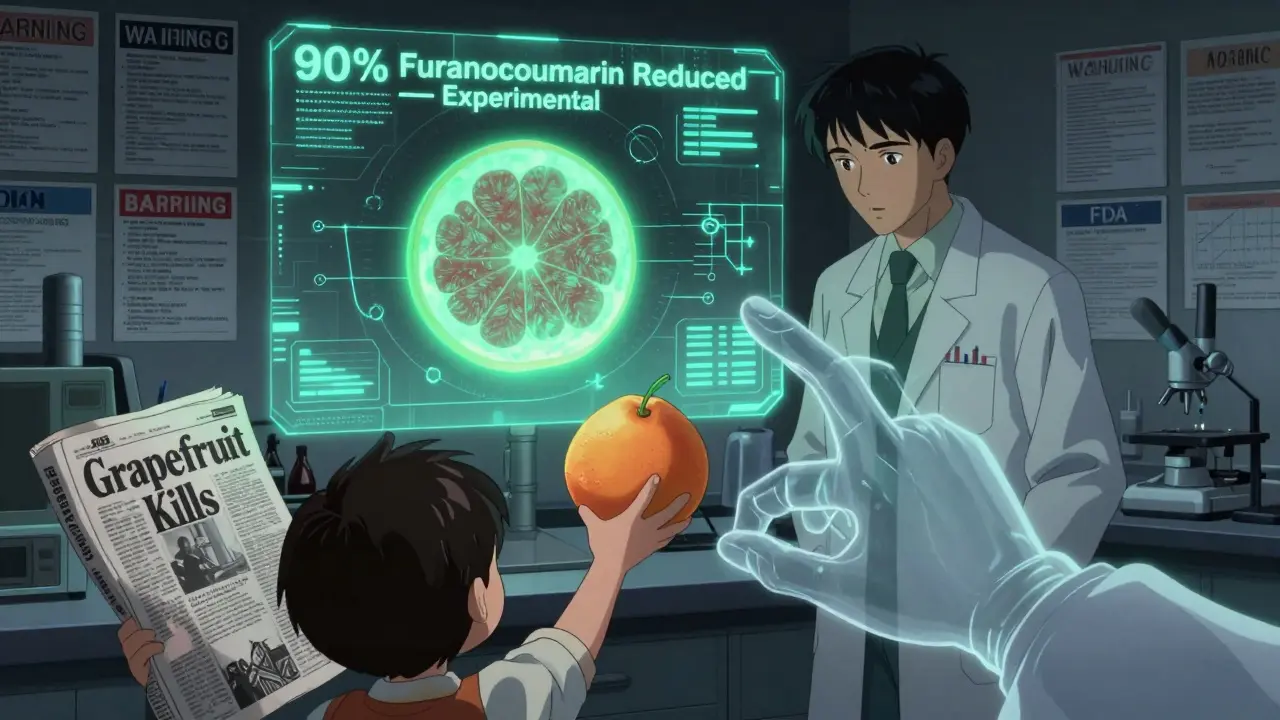
What If I Already Ate Some?
If you accidentally drank grapefruit juice and you’re on a high-risk medication, don’t panic-but don’t ignore it either. Monitor for symptoms: unexplained muscle pain or weakness (possible rhabdomyolysis), dizziness, irregular heartbeat, nausea, or swelling. Call your doctor. Don’t wait. The interaction doesn’t always cause immediate symptoms, but the damage builds up.And don’t think you can time it. Drinking juice at night and taking your pill in the morning? Doesn’t work. The enzyme stays disabled for up to three days. There’s no safe window.
What’s Changing? What’s Next?
Science is trying to fix this. In October 2023, the USDA announced CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety trials. That could mean safe grapefruit in the future. But it’s still years away from stores. Until then, the advice hasn’t changed: avoid it.Drug makers are also feeling the impact. Statin sales dropped by $1.2 billion a year after patients started avoiding grapefruit with simvastatin. But safety matters more than profits. And patient awareness? Still too low. A 2022 survey found only 38% of patients remembered being warned about grapefruit. That’s a failure in communication. You can’t rely on labels or memory. You need to ask.
Bottom Line
Grapefruit juice isn’t just a fruit. For people on certain medications, it’s a hidden hazard. It doesn’t matter if you’re young, healthy, or eat it once a week. If your drug interacts with it, one glass can be enough to cause serious harm-or death. There’s no safe amount. No timing trick. No exception.Check your meds. Talk to your pharmacist. Switch if needed. And if you’re not sure? Skip it. Your body will thank you.
Can I drink grapefruit juice if I take my medication at a different time of day?
No. Grapefruit juice disables the CYP3A4 enzyme in your gut for 24 to 72 hours. Even if you drink it at night and take your pill in the morning, the enzyme is still inactive. The interaction isn’t about timing-it’s about the lasting damage to your digestive system’s ability to process the drug. Avoid grapefruit entirely while on affected medications.
Is grapefruit juice safe with over-the-counter drugs?
Some OTC drugs can interact. Fexofenadine (Allegra), an antihistamine, is one example-grapefruit juice can reduce its absorption, making it less effective. Other OTC painkillers like ibuprofen or acetaminophen are generally safe, but if you’re taking multiple meds, including supplements, it’s best to check. Don’t assume OTC means safe with grapefruit.
Do all grapefruit varieties have the same risk?
White grapefruit has higher levels of furanocoumarins than red or pink varieties, so it’s more potent. But even red grapefruit can cause dangerous interactions. The difference isn’t enough to make red grapefruit safe. The FDA and other health agencies treat all grapefruit the same: avoid it if your medication is on the list.
Can I switch to another citrus fruit to avoid the problem?
Yes, but not all citrus is safe. Sweet oranges (navel, Valencia), lemons, and limes don’t contain furanocoumarins and are safe to consume. Seville oranges (used in marmalade) and pomelos do contain them and should be avoided. Always check the type before assuming it’s safe.
Why don’t all doctors warn patients about this?
Many do-but not all. A 2022 survey found only 38% of patients recalled being warned about grapefruit interactions. It’s often overlooked because it’s not in every drug’s headline warning, and doctors assume patients will read labels. But patients don’t always read them. The safest approach is to ask your pharmacist or doctor directly. Don’t rely on memory or assumption.
Are there any medications that are completely safe with grapefruit?
Yes. Many drugs don’t rely on CYP3A4 for metabolism. Pravastatin, rosuvastatin, atorvastatin (in small amounts), and most antibiotics, antidepressants like sertraline, and thyroid medications like levothyroxine are not affected. But you can’t assume-always check your specific medication. Even a drug that’s generally safe can have exceptions based on dosage or other factors.





Katie Taylor
December 24, 2025 AT 03:02