When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how do regulators know it really does? The answer lies in something most people never hear about: dissolution profiles. This isn’t magic or guesswork. It’s a precise, science-backed way to prove that a generic drug releases its active ingredient the same way as the original - and that’s what keeps patients safe and treatments effective.
What Dissolution Profiles Actually Measure
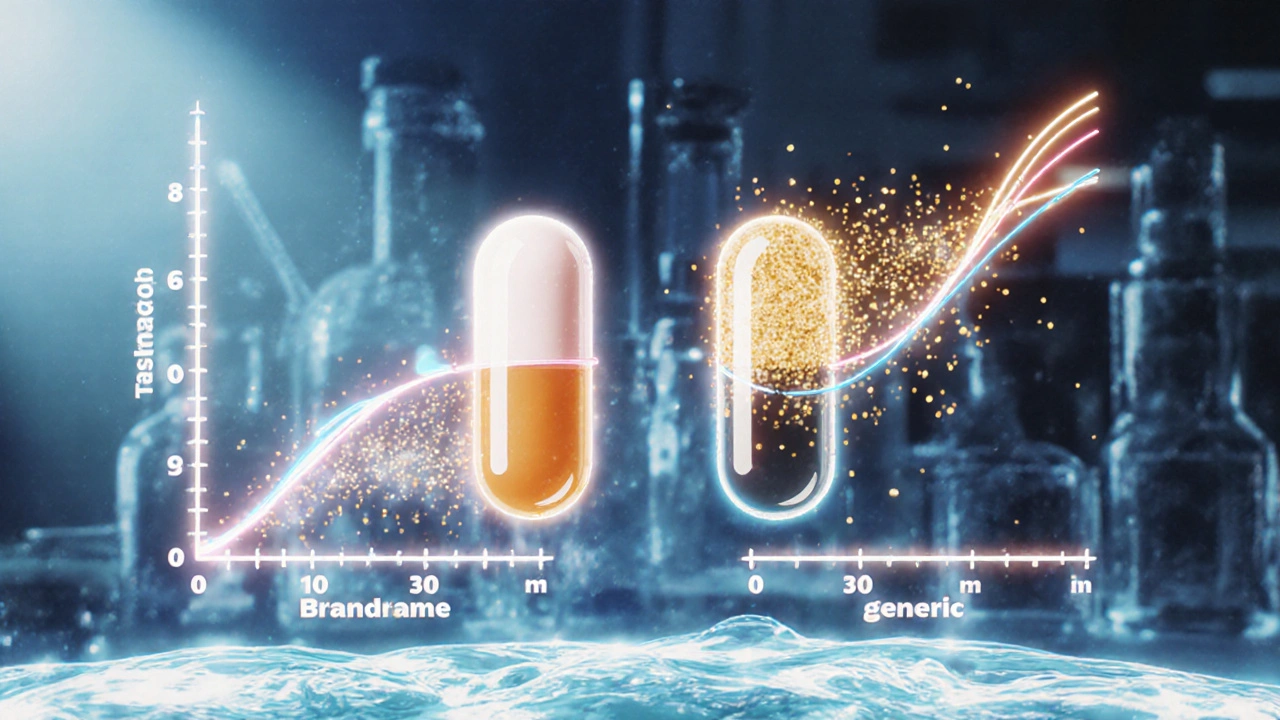
Dissolution testing simulates how a pill breaks down in your body. Imagine putting a tablet into a liquid that mimics stomach or intestinal fluid, then watching how fast the drug comes out. That’s dissolution. The results are plotted over time as a curve - the dissolution profile. For a brand-name drug, this curve is mapped during development. For a generic, the goal is to match it as closely as possible.
This isn’t just about speed. It’s about pattern. Does the drug release 20% in 15 minutes? 50% by 30 minutes? 85% by 60? If the generic’s curve looks nearly identical to the brand’s at every time point, it’s likely to behave the same in your bloodstream. That’s why regulators require this test - not just for new generics, but also when a manufacturer changes its formula, equipment, or even the color of the pill.
The f2 Similarity Factor: The Industry Standard
The most widely accepted tool for comparing these curves is the f2 factor. It’s a mathematical score between 0 and 100. A perfect match? f2 = 100. The regulatory sweet spot? Between 50 and 100. If your generic scores below 50, regulators will ask for more data - often a full bioequivalence study with human volunteers, which costs 3 to 5 times more and takes months longer.
Here’s how it works: You test 12 tablets of the brand and 12 of the generic under identical conditions - same temperature (37°C), same agitation (50-100 rpm), same pH. You measure how much drug dissolves at 10, 15, 30, 45, and 60 minutes (or until 85% is released). Then you plug those numbers into the f2 formula. The result? A single number that tells you how similar the two profiles are.
But here’s the catch: f2 isn’t foolproof. A 2014 study in Dissolution Technologies found that for some drugs, especially those with high variability, f2 can falsely approve two profiles that are actually different. One Pfizer scientist reported a case where a generic scored f2 = 49.8 - just 0.2 below the cutoff - even though it performed identically in patients. The system rejected it anyway. That’s because f2 doesn’t care about the shape of the curve, only the overall closeness. Two profiles can have the same average dissolution but release the drug in totally different ways - one fast then slow, the other steady. That’s a problem.

Why the Method Matters More Than the Number
Dr. Lawrence Yu, former FDA deputy director, put it bluntly: “f2 > 50 is necessary but not sufficient.” What does that mean? The test method itself must be good enough to detect real differences. If your dissolution method doesn’t distinguish between a well-made tablet and a flawed one, then f2 is meaningless.
That’s why regulators require the method to be “discriminatory.” Developers must prove their test can spot problems. How? By testing stressed samples - tablets that were overheated, over-compressed, or aged. If the method can’t tell the difference between a good tablet and a damaged one, it fails. A 2020 study showed this kind of method development takes 8 to 12 weeks of fine-tuning. It’s not plug-and-play.
And the media matters too. For a drug meant to dissolve in the small intestine, testing only in stomach acid (pH 1.2) won’t cut it. You need pH 4.5 and 6.8 too - especially for BCS Class I drugs (highly soluble, highly permeable). The FDA now requires similarity in all three media for biowaivers. One Teva case study showed a 25mg amlodipine tablet got approved with f2 = 63.2 in pH 6.8 - after they fixed a misaligned paddle in their dissolution apparatus. That small adjustment saved $1.2 million in testing costs.
When f2 Isn’t Enough
For drugs with high variability - like low-dose medications under 5mg - f2 often fails. A 2022 survey of 127 labs found that 73% of failed comparisons weren’t due to bad products. They were due to sloppy lab work: uncalibrated machines, inconsistent temperature, poor sample handling. In these cases, regulators look at alternatives.
One option is the Mahalanobis Distance Test (MDT). It looks at the whole profile as a shape in multi-dimensional space, not just point-by-point. A 2021 University of Maryland study found MDT correctly flagged dissimilar profiles 94% of the time, compared to 82% for f2 bootstrapping. But MDT needs specialized software and statisticians - not something every small generic maker can afford.
Another approach? Combine f2 with the area under the curve (AUC). The FDA found that using f2 ≥ 50 plus an AUC ratio between 0.80 and 1.25 made predictions of in vivo equivalence 23% more accurate than f2 alone. For high-risk drugs - like blood thinners or epilepsy meds with narrow therapeutic windows - the FDA’s 2023 draft guidance now recommends f2 ≥ 65, not 50. That’s because a small difference in absorption could mean a seizure or a bleed.
What This Means for You as a Patient
When you take a generic, you’re not gambling. Every batch has been tested. Every change - even a new supplier for the dye - triggers a new dissolution comparison. The system isn’t perfect, but it’s rigorous. And it works. In 2023, 84% of biowaiver applications based on dissolution profiles were approved by the FDA - up from 68% in 2015. That’s because labs got better, methods got smarter, and regulators stopped treating f2 as a magic number.
Here’s the bottom line: if your generic looks different - maybe it’s a different color, shape, or size - don’t worry. That doesn’t mean it’s weaker. What matters is the dissolution profile. And if it passed f2 ≥ 50 (or higher, depending on the drug), it’s been proven to behave the same way in your body.
What’s Next for Dissolution Testing
The future is getting smarter. Biorelevant media - liquids that mimic real stomach and intestine conditions - are now standard for certain drugs. Some companies are even using machine learning to predict how a dissolution curve will translate to blood levels, cutting down testing time. The FDA and EMA are working together to standardize these methods globally by 2026.
For now, the rules are clear: if you’re making or taking a generic, dissolution profiles are the invisible handshake between science and safety. They’re not flashy. They don’t make headlines. But they’re the reason you can trust that your $5 pill works just like the $50 one.
What is a dissolution profile in pharmaceuticals?
A dissolution profile is a graph that shows how much of a drug releases from a tablet or capsule over time under controlled lab conditions. It’s measured at specific time points (like 10, 30, and 60 minutes) in a fluid that mimics the human digestive system. This profile helps determine if a generic drug behaves the same way as the brand-name version before it’s ever given to a patient.
Why is f2 used to compare generic and brand drugs?
The f2 similarity factor is a mathematical tool that calculates how close two dissolution curves are. It’s used because it’s simple, widely accepted by regulators like the FDA and EMA, and correlates well with real-world performance for many drugs. An f2 score between 50 and 100 suggests the two products are similar enough that a full human study isn’t needed - saving time and money without compromising safety.
Can a generic drug with an f2 score of 48 still be safe?
Technically, an f2 score below 50 doesn’t automatically mean the drug is unsafe - but it does mean regulators won’t approve it without more evidence. A 2017 EMA paper found that 18% of products with f2 scores between 48 and 50 still worked the same in patients. But because f2 is a screening tool, not a final verdict, companies with scores below 50 must run full bioequivalence studies with volunteers to prove safety. The system is designed to be cautious.
Do all generic drugs need dissolution profile testing?
Yes - for immediate-release solid oral dosage forms (like tablets and capsules), dissolution profile comparison is required for nearly all generic applications. The FDA approved over 78% of generic drug applications in 2022-2023 based on dissolution data. Exceptions are rare and usually involve complex formulations like extended-release or injectables, which require additional testing.
How do I know if my generic drug passed dissolution testing?
You won’t see the data - it’s filed with regulators, not printed on the label. But you can trust the system: every generic approved in the U.S., EU, Canada, or Australia has passed dissolution testing. If a drug is on the market as a generic, it has met the same quality standards as the brand. The only visible sign is the lower price - proof that the system is working efficiently.
What happens if a generic drug fails dissolution testing?
If a generic fails, the manufacturer must either reformulate the product, improve the manufacturing process, or run a full bioequivalence study with human volunteers. This can delay approval by months and cost millions. In some cases, the drug never makes it to market. That’s why companies invest heavily in getting dissolution right the first time - because failure isn’t just a technical problem, it’s a financial one.
Are there drugs where dissolution testing doesn’t work well?
Yes. Drugs with very low doses (under 5mg), highly variable absorption, or poor solubility (BCS Class II and IV) are harder to test. For these, dissolution profiles may not predict in vivo performance accurately. In those cases, regulators require human bioequivalence studies instead of relying on f2 alone. That’s why not all generics can be approved via biowaiver - the science has limits.
How often are dissolution tests performed on generic drugs?
Every time there’s a manufacturing change - even switching suppliers for an inactive ingredient like cornstarch - the dissolution profile must be retested and compared to the original. Regulators require this under ICH Q8-Q11 guidelines. It’s not a one-time test. It’s an ongoing quality control process that ensures the drug you get today is the same as the one you got last year.





Shirou Spade
November 25, 2025 AT 15:54