Every year, thousands of accidental poisonings happen in homes-not because of chemicals or cleaning products, but because someone grabbed the wrong pill, took an expired one, or a child got into the medicine cabinet. In Australia, the medication storage checklist isn’t just a good idea-it’s a lifesaver. And it’s not complicated. You don’t need fancy gadgets or expensive lockboxes. You just need a clear system, a little routine, and the willingness to change old habits.
Why Your Current Medicine Cabinet Is Probably Unsafe
Most people store medications in the bathroom. It’s convenient. It’s where you brush your teeth. But it’s also the worst place in the house for pills. Showers spike humidity to 80-90%. Temperature swings from 15°C to 30°C in minutes. That’s enough to break down insulin, antibiotics, and even painkillers. Studies show medications stored in bathrooms lose up to 50% of their potency in just a few months. And it’s not just about effectiveness. The Australian Poisons Information Centre reports that over 1,200 children under five are treated each year for accidental medicine ingestion. Nearly all of them got into a cabinet that wasn’t locked. Even if you think your child can’t reach it, they can. Kids climb. They pull chairs. They open doors. A standard medicine cabinet stops only 12% of child access attempts.Core Elements of a Home Medication Storage Checklist
A real medication storage checklist isn’t a one-time task. It’s a system. Here’s what it must include.- Location: Pick a cool, dry, dark spot. A locked cabinet in a bedroom, linen closet, or hallway drawer works best. Avoid kitchens and bathrooms. Keep it out of sight and out of reach-ideally above 1.2 meters and behind three closed doors.
- Locking: Use a lockbox, padlock, or cabinet with a childproof latch. Combination locks are 34% more effective than key locks because no one forgets the code. Even if you think you’re the only one who needs access, teenagers and visitors might not be so careful.
- Separation: Keep each person’s meds on separate shelves or in labeled bins. Mixing up your blood pressure pill with your partner’s diabetes medication can be deadly. High-alert drugs like insulin, opioids, or warfarin need their own locked container with a clear “High Alert” label.
- Original Containers: Never transfer pills to pill organizers unless you’re using them daily and can refill them safely. The original bottle has the name, dosage, expiry date, and pharmacy info. Losing that info leads to mistakes.
- Refrigeration: If a medication says “store in fridge,” keep it between 2°C and 8°C. Insulin, some antibiotics, and eye drops fall into this category. But don’t store them near food. Use a small, labeled bin inside the fridge just for meds.
- Light Protection: Some drugs-like nitroglycerin or certain antibiotics-break down in light. Keep them in their original amber bottles or inside an opaque box. Sunlight can cut potency by 40% in under a month.
How to Organize for Clarity and Safety
Organization isn’t just about neatness. It’s about preventing errors. Start by emptying your current storage. Sort everything by user: “John’s meds,” “Maria’s meds,” “Kids’ meds.” Then sort by type: oral, topical, injectable, inhalers. Use small plastic bins or drawer dividers. Label each one clearly. For kids, put all topical creams, lotions, and repellents in one bin. Why? Because a 2021 FDA report found 127 cases where someone used a skin cream as an oral medicine. That’s not a typo. That’s a real, preventable mistake. For inhalers, store them in a sealed plastic bag. They’re easy to accidentally press. One accidental puff can send a child into distress. And for insulin pens, always keep the unused ones cold. Once opened, they’re good at room temperature for 14 to 56 days, depending on the brand. Write the opening date on the pen with a permanent marker.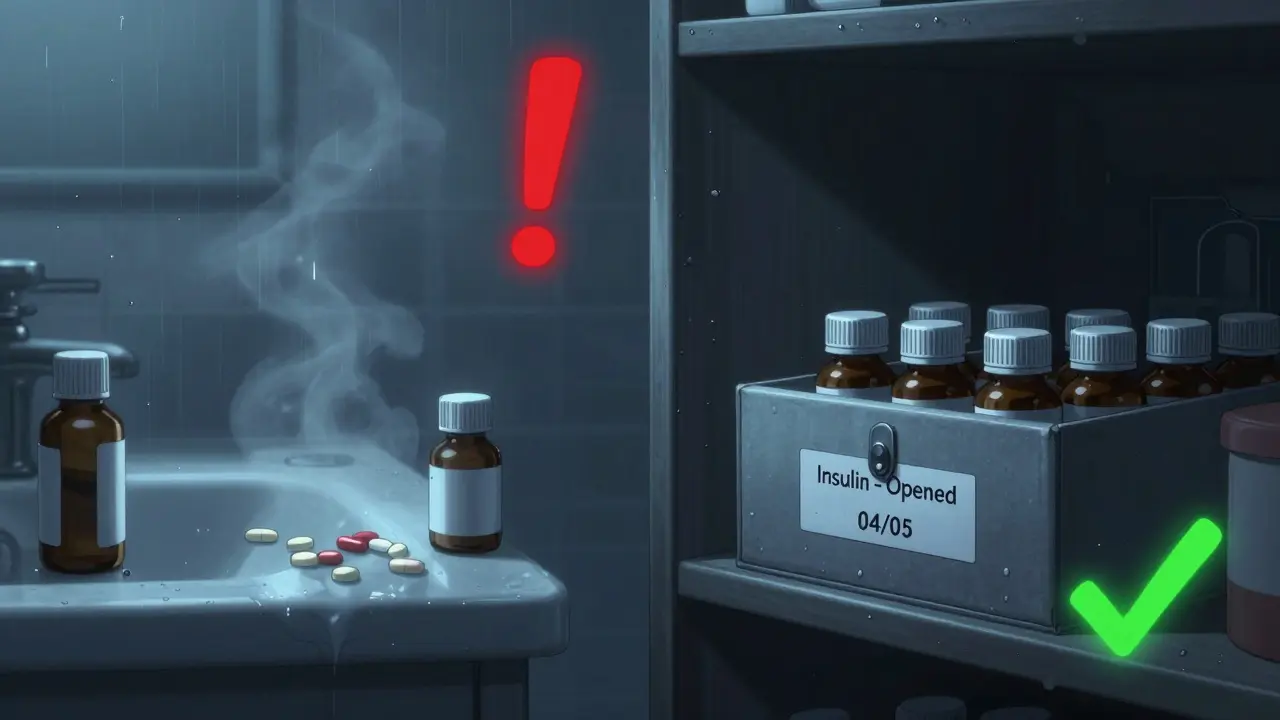
Expiration Dates and What to Do About Them
Most people don’t know that 70% of households still have expired meds lying around. And yes, they’re still active. But not always as intended. The FDA says 82% of medications retain 90% potency one year past their expiry date-if stored properly. But at three years? Only 42%. That’s not just ineffective. It’s dangerous. You might think you’re getting a full dose, but you’re not. Set a reminder: check your meds every six months. Do it in April and October, right after daylight saving changes. It’s easy to remember. Pull everything out. Look for:- Discoloration (pills turning yellow or brown)
- Cracking, crumbling, or unusual texture
- Odd smells-especially for liquids or ointments
- Expired dates
Safe Disposal: Don’t Flush or Trash
Flushing meds down the toilet or throwing them in the bin isn’t just bad for the environment-it’s risky for people and pets. A 2021 USGS study found pharmaceuticals in 80% of U.S. waterways. Australia doesn’t have perfect take-back systems yet, but we’re getting closer. Here’s what to do:- Find a pharmacy that offers a medicine return program. Many Chemist Warehouse, TerryWhite Chemmart, and independent pharmacies participate.
- If no drop-off is nearby, mix the pills with something unappetizing: coffee grounds, cat litter, or dirt. Use a 1:3 ratio. Seal it in a plastic bag. Put it in the trash.
- Remove or black out labels on bottles before recycling them. This protects your privacy.
- Never leave expired meds in an open drawer or on a counter while waiting to dispose of them. That’s when accidents happen.
Special Cases: Kids, Seniors, and High-Risk Meds
If you have young children, elderly parents, or someone on opioids, insulin, or sedatives, you need extra steps. For kids:- Store all meds-even vitamins and cough syrup-in a locked box.
- Never say “candy” when giving medicine. Kids learn fast.
- Keep a log of when you give doses. Mistakes happen when you’re tired.
- Use a pill organizer with alarms or a smart dispenser that texts you when to take it.
- Keep all meds in large-print labels. Many seniors have trouble reading small text.
- Check for duplicate prescriptions. Sometimes two doctors prescribe the same drug without knowing.
- Insulin: Refrigerate unopened. Mark opened vials with date and discard after 14-56 days.
- Opioids: Double-lock them. Even if you think you’re safe, someone else might try to take them.
- Warfarin: Keep it in a separate locked container. A wrong dose can cause internal bleeding.

Monthly and Biannual Maintenance Routines
A checklist only works if you use it. Do this every month:- Check fridge temp for meds (should be 2-8°C). Use a small thermometer.
- Look for any new pills you don’t recognize. Ask your pharmacist.
- Ensure all caps are tight and bottles are upright.
- Empty the entire storage area.
- Sort by person, type, and expiry.
- Discard expired or damaged meds properly.
- Update your list. Add new meds. Remove old ones.
- Re-lock the cabinet. Test the lock.
What to Do If Something Goes Wrong
Even with the best system, accidents happen. If a child swallows medicine:- Don’t wait. Don’t induce vomiting.
- Call the Poisons Information Centre on 13 11 26 (Australia-wide, 24/7).
- Have the pill bottle ready. They’ll ask for the name, dosage, and time ingested.
- Call your pharmacist or GP immediately.
- Don’t panic. Many accidental mix-ups are harmless if caught early.
- Update your checklist to prevent it again.
Final Thought: This Isn’t About Perfection. It’s About Prevention.
You don’t need to be a nurse to keep your family safe. You just need to be consistent. A medication storage checklist isn’t about control. It’s about care. It’s about making sure the next time someone reaches for a pill, they get the right one-safe, strong, and on time. Start small. Pick one thing: lock the cabinet. Or check the expiry dates. Do that today. Then add the next step tomorrow. In a month, you’ll wonder how you ever lived without it.Where is the best place to store medications at home?
The best place is a cool, dry, dark, and locked cabinet-like a bedroom drawer, linen closet, or hallway storage. Avoid bathrooms and kitchens because heat, humidity, and light can damage medications. Keep it out of reach of children and pets, ideally above 1.2 meters and behind closed doors.
Can I store medications in the fridge?
Only if the label says to. Insulin, some antibiotics, and eye drops need refrigeration between 2°C and 8°C. Store them in a sealed, labeled container away from food. Never store medications in the fridge door-it’s too warm and unstable. Always check the manufacturer’s instructions.
How do I know if a medication has gone bad?
Look for changes: pills that are discolored, cracked, or sticky; liquids that are cloudy or have particles; ointments that smell odd or separate. If you’re unsure, throw it out. Never take a pill that looks or smells wrong, even if it’s not expired.
What’s the safest way to dispose of expired meds?
Take them to a pharmacy that offers a medicine return program. If that’s not available, mix pills with coffee grounds or cat litter (1:3 ratio), seal them in a plastic bag, and throw them in the trash. Never flush them down the toilet or sink-this contaminates water supplies.
Should I keep all medications in their original bottles?
Yes, unless you’re using a daily pill organizer. The original bottle has the name, dosage, expiry date, and pharmacy info. If you transfer pills to another container, you risk confusion or misidentification. Always keep the label on-even if it’s faded.
How often should I check my medication storage?
Do a quick check every month: look for damaged pills, check fridge temps, and make sure everything is still locked. Do a full inventory every six months-ideally in April and October. This helps you catch expired meds before they’re taken and keeps your system running smoothly.






Dylan Smith
December 15, 2025 AT 19:55