When you pick up a prescription and see a generic version on the shelf, you might wonder: is this really the same thing? After all, it looks different, costs less, and has a different name. But here’s the truth: if it’s FDA-approved, it’s not just similar-it’s pharmaceutically equivalent. That’s not marketing jargon. It’s a strict, science-backed standard that ensures your generic drug contains the exact same active ingredient, in the exact same amount, delivered the exact same way as the brand-name version.
What Pharmaceutical Equivalence Actually Means
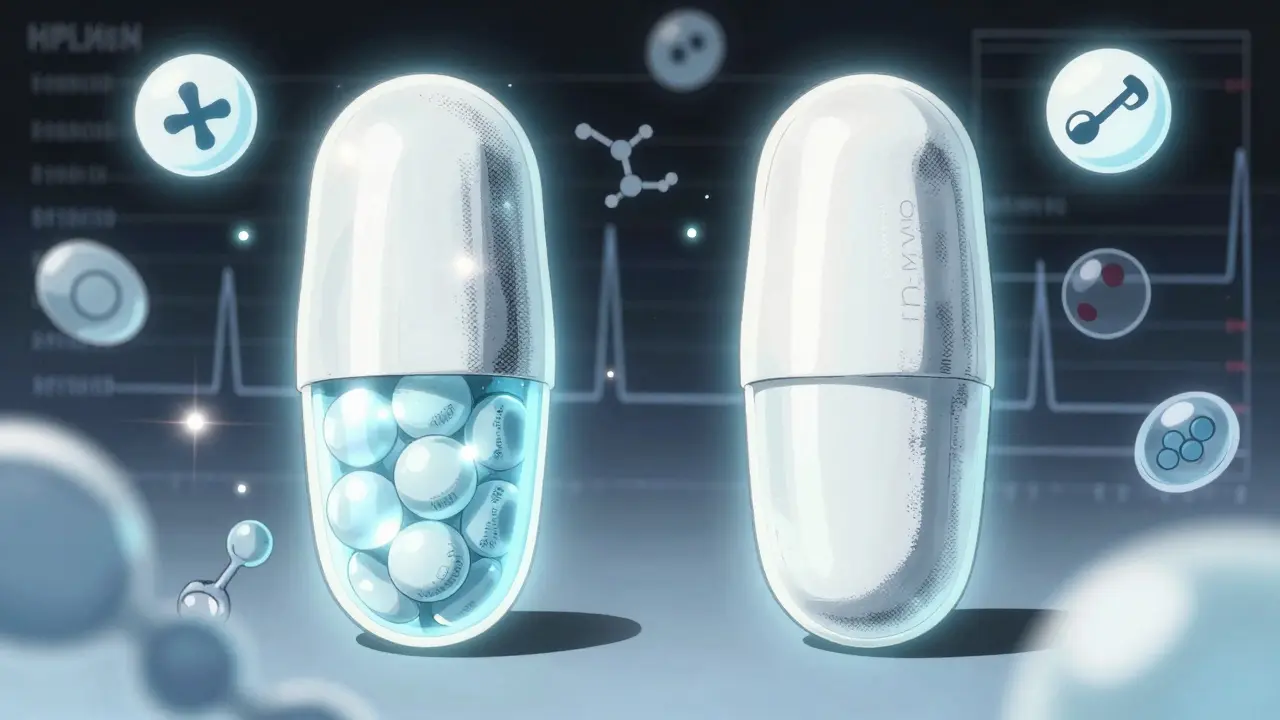
Pharmaceutical equivalence isn’t about how the pill looks or tastes. It’s about what’s inside. According to the FDA’s official definition, two drugs are pharmaceutically equivalent if they have:- The same active ingredient (no more, no less)
- The same dosage form (tablet, capsule, injection, etc.)
- The same route of administration (swallowed, injected, applied to skin)
- The same strength (e.g., 10 mg, 500 mg)
- The same quality, purity, and identity standards
That’s it. No wiggle room on the active ingredient. If the brand-name drug has 25 mg of lisinopril, the generic must have exactly 25 mg-no 20 mg, no 30 mg. The FDA requires analytical testing using methods like high-performance liquid chromatography (HPLC) to confirm this. The active ingredient must be within ±5% of the labeled amount. That’s tighter than most food nutrition labels.
What’s allowed to differ? Everything else. Color, shape, size, flavor, packaging, and even the inactive ingredients (called excipients) can change. That’s why your generic metformin might be a white oval pill instead of a blue round one. Those differences don’t affect how the drug works in your body. They’re just for branding, cost, or manufacturing reasons.
Why This Matters More Than You Think
You might think, “If it’s the same active ingredient, why does it matter?” Because pharmaceutical equivalence is the first and non-negotiable step before a generic drug can even be considered safe to use. It’s the foundation. Without it, nothing else matters.Before 1984, generic drugs were often unreliable. Manufacturers didn’t have to prove anything. The Hatch-Waxman Act changed that. It created the Abbreviated New Drug Application (ANDA) process, which lets generic companies skip expensive clinical trials-but only if they prove pharmaceutical equivalence. That’s how we got to the point where 90% of prescriptions in the U.S. are filled with generics today.
And the savings? Real. From 2009 to 2023, generics saved the U.S. healthcare system over $2.2 trillion. The average prescription saves $1,008 when you choose generic over brand. That’s not just a discount-it’s access to medicine for millions who couldn’t otherwise afford it.
Pharmaceutical Equivalence ≠ Therapeutic Equivalence
Here’s where people get confused. Just because two drugs are pharmaceutically equivalent doesn’t mean they’re interchangeable in every situation. That’s where bioequivalence and therapeutic equivalence come in.Pharmaceutical equivalence says: “Same ingredients, same amount.”
Bioequivalence says: “Same amount gets into your bloodstream at the same speed.”
Therapeutic equivalence says: “Same effect, same side effects.”
The FDA uses a three-tiered system. Pharmaceutical equivalence is Step One. Bioequivalence is Step Two. Therapeutic equivalence is Step Three.
Bioequivalence is measured by comparing how much of the drug enters your blood (AUC) and how fast it peaks (Cmax). The FDA allows a range of 80% to 125% compared to the brand-name drug. That sounds wide-but it’s based on decades of data showing that within this range, clinical outcomes are virtually identical for most drugs.
But here’s the catch: for drugs with a narrow therapeutic index-like warfarin, lithium, or levothyroxine-those small differences in absorption can matter. A 5% change in blood levels might mean a blood clot or a seizure. That’s why the FDA rates these drugs more carefully. In the 2024 Orange Book, only 12,845 out of 15,372 generic drugs are rated “AB,” meaning they’re therapeutically equivalent. The rest are rated “BX” or “BZ,” meaning they’re not automatically interchangeable.
What Happens When Excipients Cause Problems
You might hear stories about people reacting to generics. It’s rare-but it happens. And it’s not because the active ingredient is different. It’s because of the fillers.Excipients like dyes, lactose, gluten, or preservatives can trigger reactions in sensitive patients. A 2022 survey found that 87% of pharmacists had seen at least one patient have a minor side effect-like a rash or stomach upset-due to a change in excipients. Only 2.3% of those patients needed to switch back to the brand.
If you have allergies, celiac disease, or sensitivities, always check the inactive ingredients. The FDA doesn’t require full disclosure on the label, but pharmacists can access the full formulation through the Orange Book or manufacturer data. Ask your pharmacist if you’re unsure.
What You Should Know Before Taking a Generic
You don’t need to be a scientist to make smart choices. Here’s what to do:- Ask your doctor if your drug has a narrow therapeutic index. If it does, ask whether the generic you’re being given is rated “AB” in the Orange Book.
- If you switch generics and notice new side effects, don’t assume it’s “not working.” Talk to your pharmacist. It might be a different excipient.
- Don’t believe the myth that generics contain only 80% of the active ingredient. That’s the bioequivalence range for how your body absorbs it-not what’s in the pill.
- Use the FDA’s Orange Book online (or ask your pharmacist) to check the therapeutic equivalence rating of your drug. Look for “AB.”
- If your insurance forces a switch and you’re worried, ask for a prior authorization for the brand. It’s your right.
What’s Changing in 2026 and Beyond
The rules aren’t static. The FDA is updating how it evaluates complex generics-like inhalers, injectables, and topical creams-where the delivery system matters as much as the drug itself. New tools like Raman spectroscopy and X-ray diffraction are being tested to better analyze the physical structure of these drugs.In 2023, the FDA launched its Complex Generic Drug Product Development program to improve standards. And in May 2024, they proposed new rules requiring more detailed testing for drugs where excipients affect how the drug works.
Meanwhile, the American Society of Health-System Pharmacists is pushing for clearer labeling of inactive ingredients. If you’re someone who’s had a reaction before, you’ll want to keep an eye on this.
Bottom Line: Generics Are Safe-But Stay Informed
Pharmaceutical equivalence is one of the most successful public health policies in modern medicine. It’s why you can get your blood pressure medication for $4 instead of $400. It’s why millions of people with diabetes, heart disease, or depression can afford to stay on their meds.But it’s not magic. It’s science. And like any science, it has limits. For most drugs, generics are just as good. For a few, you need to be more careful. Know your drug. Know your body. Talk to your pharmacist. And don’t let fear of the unknown keep you from saving money-or worse, skipping your medicine.
Are generic drugs really as strong as brand-name drugs?
Yes. By law, generics must contain the exact same active ingredient in the exact same amount as the brand-name version. The FDA requires analytical testing to prove this-usually within ±5% of the labeled strength. The difference in price comes from lower marketing and development costs, not weaker ingredients.
Why do generic pills look different from brand-name ones?
The law allows generic manufacturers to change the color, shape, size, and packaging to avoid infringing on the brand’s trademark. These differences don’t affect how the drug works. The active ingredient is identical. The changes are purely cosmetic or for manufacturing efficiency.
Can I switch between different generic brands safely?
For most drugs, yes. If both generics are rated "AB" in the FDA’s Orange Book, they’re considered therapeutically equivalent. But for drugs with a narrow therapeutic index-like warfarin or thyroid meds-some doctors prefer to stick with one brand to avoid tiny variations in absorption. Always check with your pharmacist if you’re switching between generics.
Do generics take longer to work than brand-name drugs?
No. Bioequivalence testing ensures that generics release the active ingredient into your bloodstream at the same rate and to the same extent as the brand-name drug. The 80%-125% range used in testing accounts for normal biological differences between people-not delays in action. If you feel a difference, it’s likely psychological or due to excipients, not speed of action.
What does "AB" mean on the FDA Orange Book?
"AB" means the generic drug has been evaluated and found to be both pharmaceutically and bioequivalent to the brand-name drug. It’s rated as therapeutically equivalent and can be substituted without concern. "BX" or "BZ" ratings mean the drug is not considered interchangeable, usually due to issues with absorption or delivery.
Should I avoid generics if I have allergies?
Not necessarily. The active ingredient is the same. But if you’re allergic to certain excipients-like lactose, dyes, or gluten-you should ask your pharmacist for the full list of inactive ingredients in the generic version. Some generics use different fillers than the brand. Switching to a different generic or the brand may be necessary if you react.
Pharmaceutical equivalence isn’t just a regulatory box to check. It’s the reason millions of people can afford to live longer, healthier lives. Understanding it helps you make smarter choices-not just about cost, but about your health.





Donny Airlangga
January 8, 2026 AT 00:17