When you pick up a generic pill at the pharmacy, you’re not just saving money-you’re trusting a system that doesn’t require the same clinical testing as brand-name drugs. That’s not a flaw. It’s by design. But it does mean the real safety check happens after the drug hits the shelves. This is where post-market studies and clinical follow-up become critical.
Why Generic Drugs Don’t Get the Same Pre-Approval Testing
Generic drugs don’t need to repeat the massive clinical trials that brand-name drugs go through. Instead, they must prove they’re bioequivalent-meaning they deliver the same amount of active ingredient into your bloodstream at the same rate as the original. The FDA approves them based on this, not on new safety data from thousands of patients. That’s efficient. It’s also risky. Clinical trials for generics usually involve fewer than 5,000 people, mostly healthy adults. They rarely include older patients, kids, pregnant women, or people with multiple chronic conditions. These are the groups who end up taking most generics. So, what happens when a drug that worked fine in a trial starts causing problems in a 72-year-old with kidney disease? That’s when post-market surveillance kicks in.The Hidden Gaps in Generic Drug Safety
A 2021 study in JAMA Internal Medicine found that 68% of serious adverse events linked to cardiovascular generics weren’t listed on the drug label when it was approved. That’s not because manufacturers hid data. It’s because the data didn’t exist yet. Side effects only show up when millions of people take a drug over years-not in a controlled 6-month trial. Some issues are subtle. A tablet might dissolve too slowly in one manufacturer’s version, leading to lower absorption. Another might release the drug too fast, causing spikes in blood levels. For drugs with a narrow therapeutic index-like levothyroxine, warfarin, or seizure meds-these tiny differences can mean the difference between control and crisis. Pharmacists on Reddit have reported multiple cases where patients developed palpitations or anxiety after switching from one generic brand of levothyroxine to another. The active ingredient is the same. But the fillers, coatings, and manufacturing processes aren’t. And for some people, those differences matter.How the FDA Tracks Generic Drug Safety After Launch
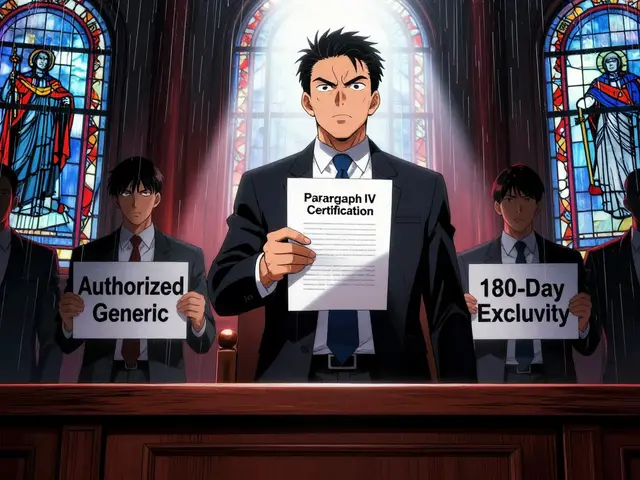
The FDA doesn’t just wait for complaints. It actively hunts for signals. Its Sentinel Initiative, launched in 2008 and fully live by 2016, scans electronic health records from over 300 million patients. It looks for patterns: spikes in hospitalizations, unusual lab results, or clusters of side effects tied to specific generic brands. Doctors and patients report problems through MedWatch, the FDA’s voluntary reporting system. In 2022, 1,247 generic drug recalls happened in the U.S.-78% of all drug recalls that year. Many were due to quality issues: tablets crumbling, liquid suspensions forming clumps, transdermal patches falling off before the drug was fully delivered. Manufacturers are legally required to report serious adverse events within 15 days. But here’s the catch: most reports don’t say which generic brand the patient took. Only 35% of reports in 2022 named the manufacturer. That makes it hard to know if the problem is with one company’s version-or if it’s a class-wide issue.
Who’s Responsible for Monitoring?
Every generic drug maker must have a pharmacovigilance system. That means staff trained to collect, review, and report adverse events. The median cost? $1.2 million per company per year. Small manufacturers struggle with this. Many still rely on manual reviews. The top 20 generic companies use AI tools to scan reports for early warning signs. Smaller ones? They’re often playing catch-up. The FDA doesn’t just review reports. It runs targeted safety reviews. In 2022, they conducted 328 of them-up 27% since 2019. Most focused on complex generics: inhalers, injectables, patches, and drug-device combos. These are harder to replicate. A slight change in the inhaler’s propellant or the patch’s adhesive can alter how much drug gets into the body. In 2021, Teva received a warning letter from the FDA for failing to report adverse events properly. Their new product approvals were delayed for six months. That’s not an outlier. It’s a signal: the FDA is watching.The Real-World Impact: Patients and Providers
A 2022 survey of 1,500 U.S. physicians found that 42% had seen possible differences in how patients responded to different generic versions of the same drug-especially with narrow therapeutic index medications. But only 18% filed formal reports. Why? Time. Bureaucracy. Uncertainty. Many doctors assume it’s just patient variability. Patients, meanwhile, rarely know which manufacturer made their pill. The label just says “metformin” or “amlodipine.” If they feel worse after a refill, they might blame their condition, not the drug. Only when they switch back and notice a pattern do they speak up. But the flip side? Cost. A 2023 Kaiser Family Foundation study showed that 89% of patients switching to generics for hypertension or diabetes reported no issues. For millions, generics mean they can afford their meds. That’s a win.
What’s Changing in 2025 and Beyond
The FDA’s 2024-2026 plan calls for product-specific surveillance plans for high-risk generics by 2025. That means instead of treating all metformin the same, they’ll track each brand’s safety profile separately. They’re also expanding the Sentinel system to include social determinants of health-like income, housing, and access to food. Why? Because a patient skipping meals might react differently to a generic drug than someone eating regularly. Real-world data matters. Pilot programs are testing blockchain to track each batch of generic drugs from factory to pharmacy. If a problem arises, they can trace it to one plant, one batch, one batch of filler. That could cut down confusion and recalls. The Generic Drug User Fee Amendments (GDUFA) III, launched in 2023, allocated $15 million specifically to boost generic safety monitoring. That’s a start. But with over 100 manufacturers and 10,000 generic products on the market, it’s still a race against scale.What You Can Do
If you take a generic drug and notice new side effects after switching brands:- Write down the exact name on the bottle (manufacturer and lot number if visible)
- Don’t assume it’s “all the same”
- Talk to your pharmacist-they can tell you which company made your pills
- Report it to MedWatch through the FDA website
Bottom Line
Generic drugs are safe for most people. They’ve saved billions in healthcare costs. But safety doesn’t end at approval. It’s an ongoing process-watching, listening, adapting. The system isn’t perfect. Reporting is messy. Attribution is hard. But it’s improving. And your awareness helps make it better.Are generic drugs less safe than brand-name drugs?
Not inherently. Generic drugs must meet the same quality, strength, and purity standards as brand-name drugs. The difference is in the testing: generics are approved based on bioequivalence, not new clinical trials. That means rare or long-term side effects may not be known until after millions of people start using them. Post-market surveillance fills that gap.
Why do some people feel different on a generic version?
The active ingredient is identical, but fillers, coatings, and manufacturing methods can vary. For drugs with a narrow therapeutic index-like thyroid meds, blood thinners, or seizure drugs-tiny differences in how fast the drug is absorbed can lead to noticeable changes in how you feel. This isn’t always a safety issue, but it can be a dosing issue.
How does the FDA know if a generic drug is unsafe after it’s on the market?
The FDA uses multiple tools: patient and provider reports through MedWatch, analysis of electronic health records via the Sentinel Initiative, targeted safety reviews, and data mining of adverse event databases. They look for unusual patterns-like a spike in liver injuries tied to a specific generic brand-that wouldn’t show up in small clinical trials.
Can I find out which company made my generic drug?
Yes. The manufacturer’s name is usually printed on the pill bottle or packaging. If it’s not clear, ask your pharmacist. They can tell you the brand and lot number. Keeping track of this helps if you notice side effects after switching refills.
What should I do if I think a generic drug is causing side effects?
First, don’t stop taking it without talking to your doctor. Then, document what you’re experiencing-when it started, what you were taking, and whether it changed after switching brands. Report it to the FDA through MedWatch online. Even one report can help. If multiple people report the same issue, the FDA may investigate further.
Are there more recalls for generic drugs than brand-name drugs?
In 2022, 78% of all drug recalls in the U.S. were for generic drugs. That’s not because generics are inherently riskier-it’s because there are far more generic products on the market (over 10,000) compared to brand-name drugs. Also, quality issues like inconsistent dissolution or packaging flaws are more common in generics due to lower profit margins and complex manufacturing processes.




Praseetha Pn
January 17, 2026 AT 18:06