Tentative Approval and Litigation: How Generic Drug Makers Wait for Market Entry
February 3 2026Fracture Risk: What Medications and Health Factors Really Increase Your Chance of Breaking a Bone
When we talk about fracture risk, the likelihood of a bone breaking due to weakness, trauma, or medication side effects. Also known as bone fragility, it’s not just something that happens to older people—it’s often driven by things you can control, like the drugs you take or how you store them. Many people don’t realize that common prescriptions—like blood pressure meds, steroids, or even some antidepressants—can quietly weaken bones over time. This isn’t theory. Studies show that long-term use of certain antihypertensives increases fall-related fractures in seniors by up to 30%, not because they cause dizziness alone, but because they also reduce bone density.
That’s why medication side effects, unintended physical changes caused by drugs, even when taken correctly. Also known as adverse drug reactions, it matters more than you think. For example, proton pump inhibitors (PPIs) used for heartburn can block calcium absorption if taken for years. Corticosteroids, often prescribed for asthma or arthritis, accelerate bone loss. Even some diabetes drugs like thiazolidinediones have been linked to higher fracture rates in women. These aren’t rare side effects—they’re well-documented, and they’re often ignored because the patient feels fine otherwise. But bones don’t complain until they break.
Then there’s bone health, the overall strength and density of your skeletal system, influenced by diet, activity, and medication use. Also known as skeletal integrity, it isn’t just about calcium and vitamin D. It’s about how you store your pills. If you keep your meds in a humid bathroom, heat can degrade them—making them less effective at protecting your bones. And if you’re managing multiple prescriptions without clear labeling, you might accidentally skip doses of your bone-strengthening drugs. That’s a silent multiplier for fracture risk.
osteoporosis, a condition where bones become porous and fragile, increasing the chance of fractures from minor falls or even coughing. Also known as brittle bone disease, it is the biggest medical cause of fracture risk in adults over 50. But it’s not inevitable. Many people with osteoporosis never break a bone because they catch it early, adjust their meds, and take simple steps—like removing tripping hazards at home or switching to a safer blood pressure drug. The problem isn’t the disease itself. It’s that most people don’t connect their daily pill routine to their long-term bone safety.
And for older adults, elderly fall risk, the chance of losing balance and falling, often worsened by dizziness from medications or poor vision. Also known as fall susceptibility in seniors, it turns small weaknesses into big breaks. A hip fracture in someone over 65 can change their life forever. But here’s the thing: many of the drugs that cause dizziness—like blood pressure pills taken at the wrong time—are the same ones that also weaken bones. It’s a double hit. Fix one, and you might fix both.
What you’ll find below are real, practical guides—no fluff—on how your meds, storage habits, and daily routines directly affect your fracture risk. From how to spot dangerous drug interactions to why your pill bottle in the bathroom is a hidden danger, these posts give you the tools to protect yourself before the break happens.
 27 Nov
27 Nov
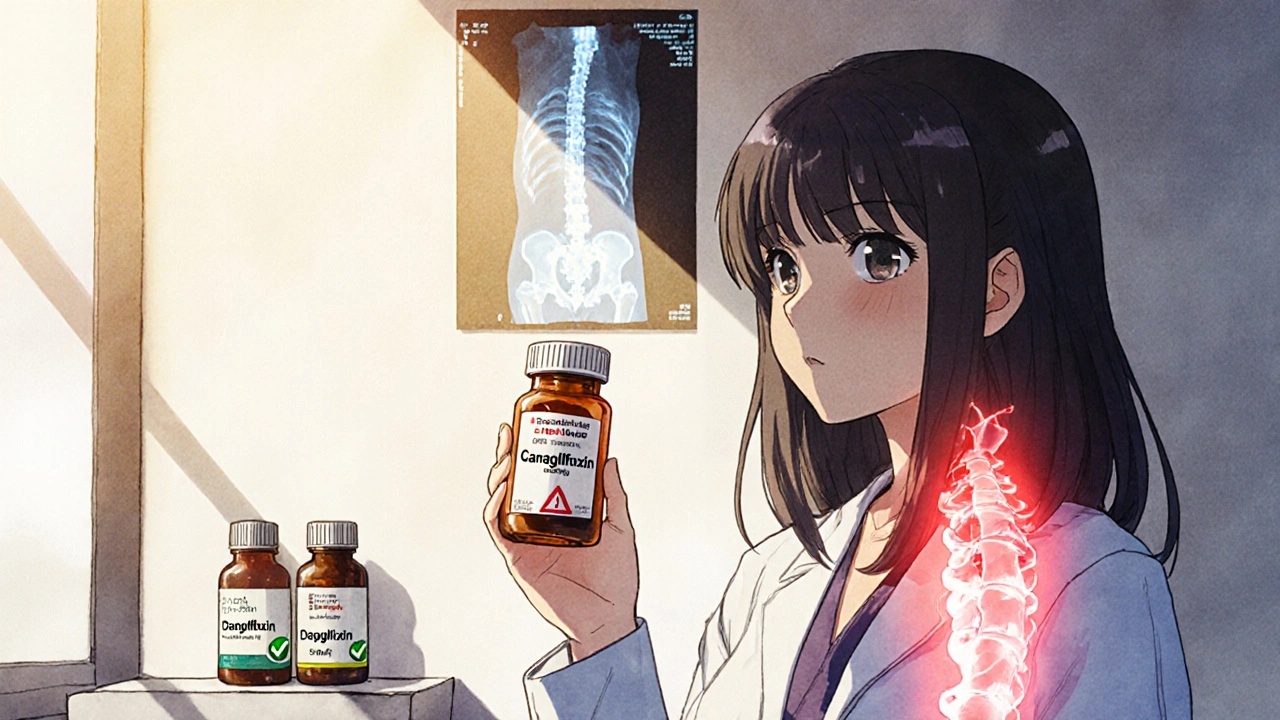
SGLT2 Inhibitors and Bone Health: What You Need to Know About Fracture Risk
SGLT2 inhibitors help manage diabetes and protect the heart and kidneys, but canagliflozin may slightly increase fracture risk in vulnerable patients. Empagliflozin and dapagliflozin show no such risk. Know your drug, assess your bone health, and make an informed choice.
Read More...