Bursitis and Posture: Causes, Effects, and Effective Relief Strategies
October 7 2025Vaginal Yeast Infection: Causes, Treatments, and What Actually Works
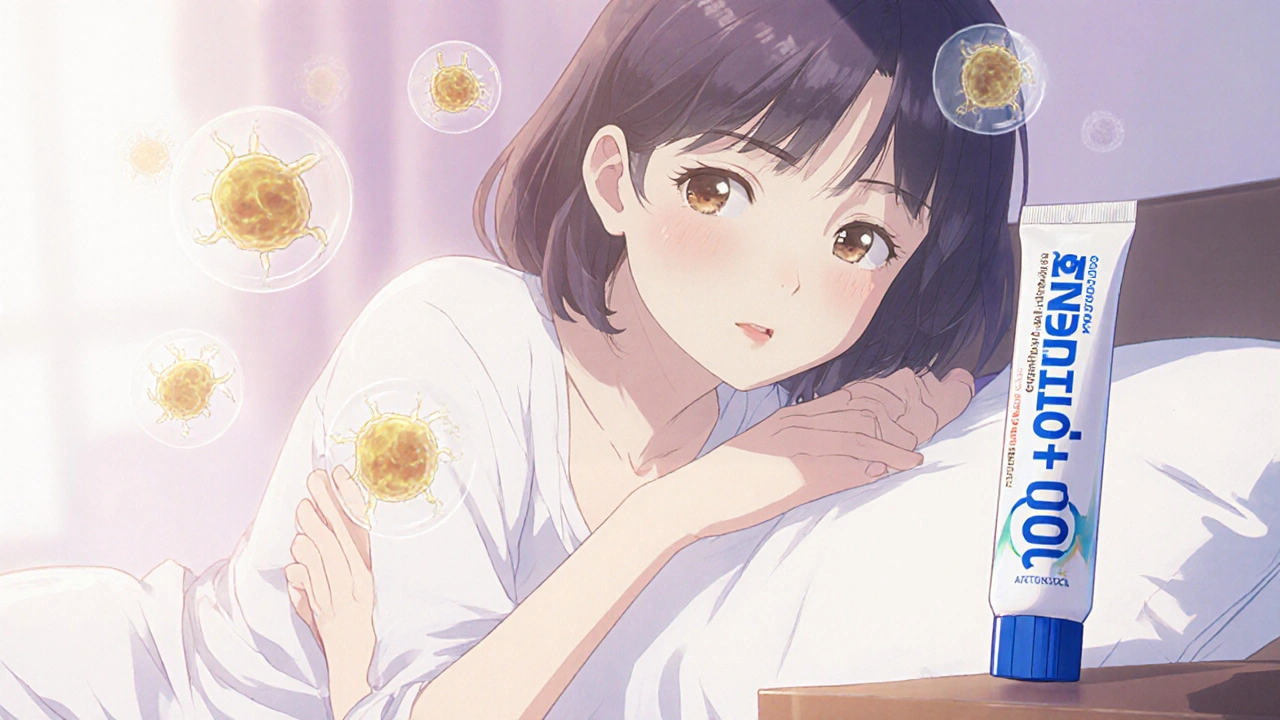
When you feel itching, burning, and thick white discharge, it’s often a vaginal yeast infection, a common fungal infection caused by an overgrowth of Candida albicans, a yeast naturally present in the vaginal microbiome. Also known as candidiasis, it affects up to 75% of women at least once in their lifetime. This isn’t a sign of poor hygiene—it’s a balance issue. Your body normally keeps yeast in check with good bacteria, but things like antibiotics, hormonal changes, or even tight clothing can tip the scales.
Many people assume all vaginal discomfort means a yeast infection, but symptoms can overlap with bacterial vaginosis or STIs. The real tell? Intense itching, swelling, and cottage-cheese-like discharge without a strong odor. If you’ve had one before and recognize the signs, an OTC antifungal cream or pill might help. But if it’s your first time, or if symptoms stick around after treatment, see a provider. Misdiagnosing can delay real care.
Antibiotics are the biggest trigger—especially broad-spectrum ones like amoxicillin or doxycycline. They wipe out good bacteria, letting yeast take over. Birth control pills, pregnancy, and uncontrolled diabetes also raise your risk. Even sugar-heavy diets can feed yeast growth, though the science here isn’t rock-solid. What’s clear? Wearing cotton underwear, avoiding douches, and changing out of wet swimsuits fast helps. And no, yogurt on the vulva won’t fix it—though eating it might help your gut flora.
There’s a lot of noise out there about natural cures—tea tree oil, garlic inserts, probiotic suppositories. Some studies show promise, but most aren’t reliable enough to trust alone. Prescription antifungals like fluconazole or clotrimazole have decades of proven results. If you keep getting infections—four or more a year—you might have recurrent candidiasis. That’s when doctors look deeper: immune issues, undiagnosed diabetes, or even resistant yeast strains.
What you’ll find below are real, practical guides from women who’ve been there. We’ve pulled together posts that break down how antifungal meds work, what to avoid when treating a yeast infection, how antibiotics and hormonal changes connect to outbreaks, and even how some alternative therapies are being studied for support. No fluff. No hype. Just clear, fact-based info to help you understand what’s happening and how to move forward.
 21 Oct
21 Oct
Gyne-Lotrimin (Imidazole) vs. Top Alternatives - In‑Depth Comparison
A clear, side‑by‑side comparison of Gyne‑Lotrimin (Imidazole) versus common antifungal alternatives, with pros, cons, dosing, and safety tips.
Read More...




