When you have G6PD deficiency, a simple prescription can turn dangerous. It’s not about being allergic or sensitive-it’s about your red blood cells lacking the tools to handle certain chemicals. This isn’t rare. Around 400 million people worldwide have it. In some parts of Africa, one in five people carries the gene. In Southeast Asia and the Mediterranean, it’s just as common. And yet, most people don’t know they have it until something goes wrong-like a fever after taking a common painkiller or an infection treated with an antibiotic that triggers a sudden drop in hemoglobin. Hemoglobin can crash from normal levels to life-threatening lows in less than a week. That’s not a side effect. That’s hemolysis. And it’s preventable.
What Happens in Your Blood When You Have G6PD Deficiency
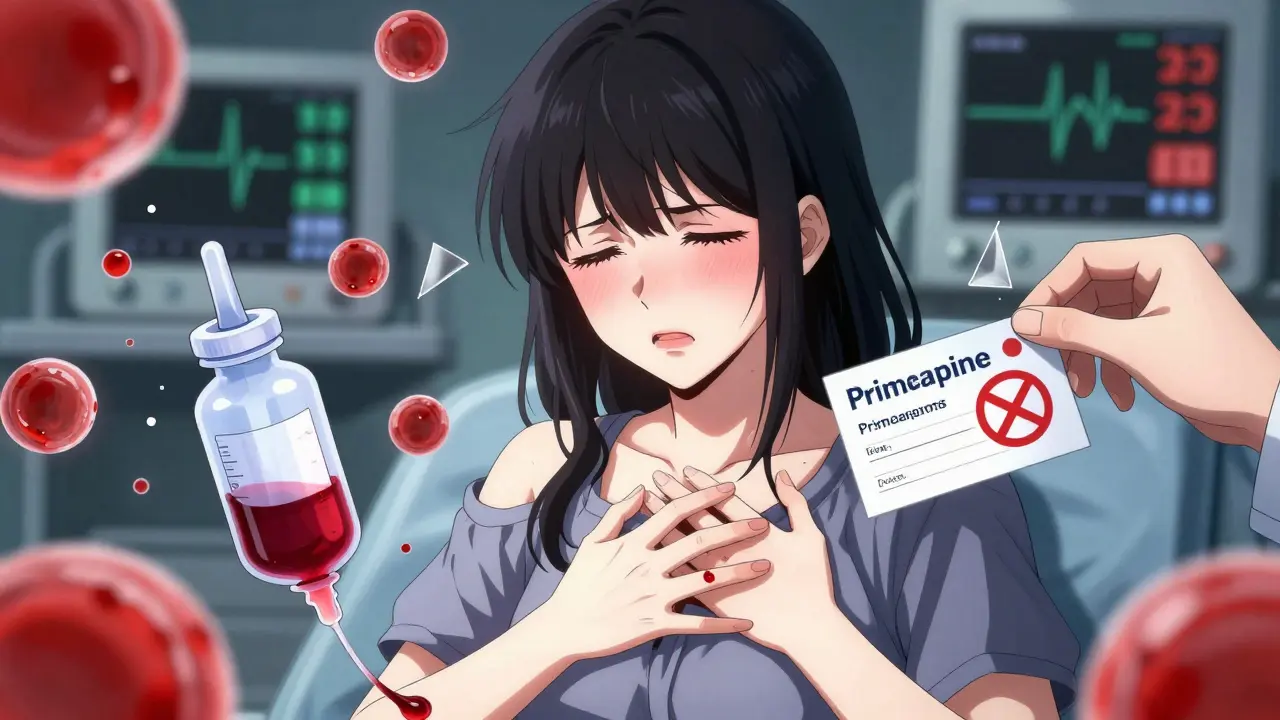
Your red blood cells are like tiny oxygen delivery trucks. They need protection from oxidative damage-basically, rust from inside your body. Glucose-6-phosphate dehydrogenase (G6PD) is the enzyme that keeps those trucks from breaking down. Without enough of it, your red cells can’t fight off stress from certain drugs, foods, or infections. The result? They burst open. That’s hemolysis. It’s not slow. It’s fast. And it can leave you pale, fatigued, with dark urine, and in severe cases, in the hospital needing blood transfusions.
There are over 200 known variants of G6PD deficiency, grouped into five classes. Most people fall into Class III-moderate deficiency. That’s the most common type globally. But even this "mild" form can cause serious problems with the wrong medication. Class II is more severe and common in Mediterranean populations. Class I is rare but dangerous, with chronic hemolysis even without triggers. The key point: no matter the class, if you’re exposed to the wrong drugs, your red cells are at risk.
Medications That Can Trigger Hemolysis
There are 87 medications on the WHO’s Essential Medicines List that are known to cause hemolysis in G6PD-deficient people. But only a few are common enough to cause real-world harm. Here are the big ones:
- Rasburicase-Used to treat tumor lysis syndrome in cancer patients. The FDA issued a Black Box Warning in 2023: this drug causes 100% hemolysis in G6PD-deficient individuals. One case reported in the American Journal of Emergency Medicine involved a 28-year-old who received rasburicase without testing. His hemoglobin dropped to 3.1 g/dL. He needed 10 units of blood.
- Methylene blue-Given for methemoglobinemia, a condition where blood can’t carry oxygen properly. But in G6PD-deficient people, it causes severe hemolysis in 95% of cases. A nurse on Reddit described giving methylene blue to a 42-year-old man who hadn’t been tested. His hemoglobin fell from 14.2 to 5.8 in 48 hours. He needed three blood transfusions.
- Primaquine-Used to treat malaria, especially to kill dormant liver stages of Plasmodium vivax. WHO guidelines say it causes 100% hemolysis in Class I and II patients. In Thailand, after making G6PD testing mandatory before prescribing primaquine, hemolytic crises dropped from 15.2% to 0.3% in just four years.
- Dapsone-Used for leprosy and some skin conditions. At doses above 50mg daily, it causes hemolysis in 80% of deficient individuals.
- Sulfonamides-Including trimethoprim-sulfamethoxazole (Bactrim). While not as dangerous as the others, they still carry risk, especially in high doses or in people with Class II deficiency.
Here’s what’s surprising: many of these warnings are ignored. A 2022 survey of 1,247 G6PD-deficient patients found that 68% had experienced at least one hemolytic episode. And 42% said their doctors didn’t even know about the drug restrictions.
Safe Alternatives to Avoid Hemolysis
You don’t have to go without treatment. Safe alternatives exist for almost every high-risk medication.
- For malaria prevention: Use atovaquone-proguanil (Malarone) instead of primaquine. The CDC says 95% of G6PD-deficient travelers using Malarone avoid hemolysis.
- For radical cure of P. vivax: Tafenoquine is now approved-but only if you’ve been tested. It’s more effective than primaquine, but the FDA requires a G6PD test before prescribing it.
- For malaria treatment: Artemisinin-based combination therapies (like artemether-lumefantrine) are safe in all G6PD deficiency classes.
- For pain and fever: Acetaminophen (paracetamol) is safe. Avoid aspirin and other NSAIDs like ibuprofen unless you’re sure your deficiency is very mild (Class IV).
- For methemoglobinemia: Instead of methylene blue, use ascorbic acid (vitamin C) or exchange transfusion if severe.
One of the biggest wins in recent years is the FDA’s 2022 requirement that rasburicase can’t be given without G6PD testing. That’s a step forward. But it’s still not standard everywhere.
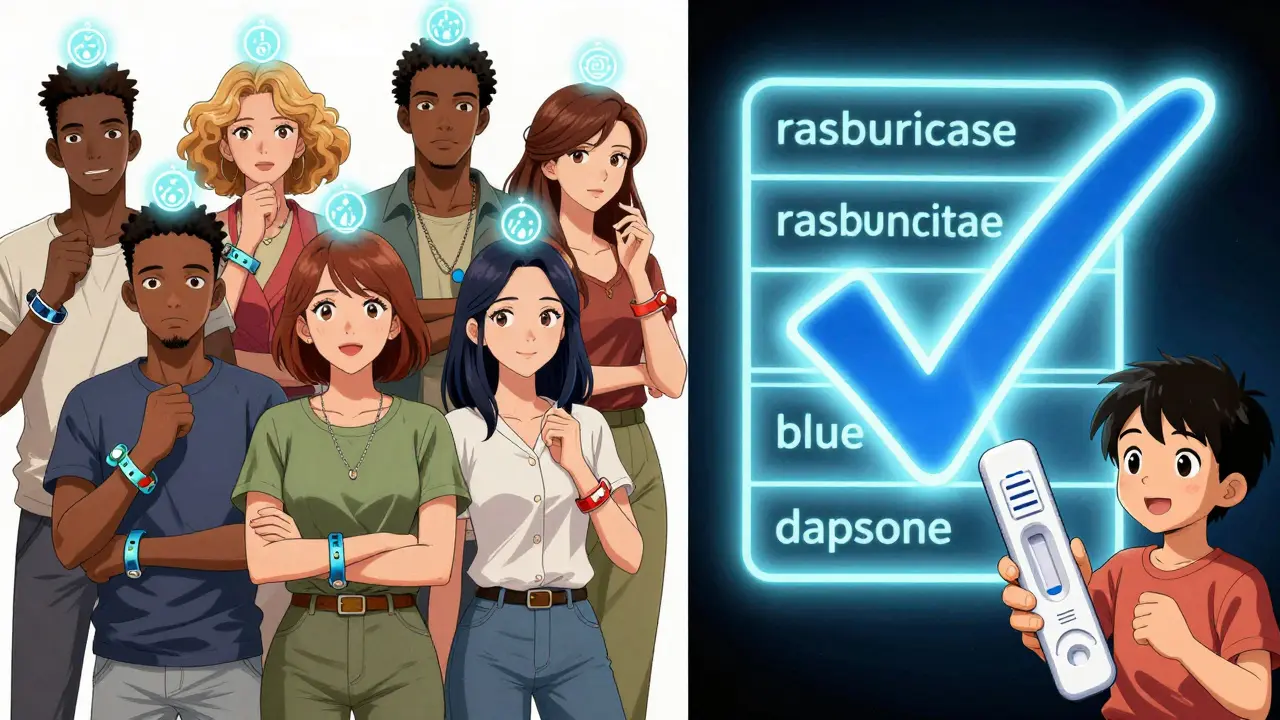
Testing: When and How
The biggest problem? Most people don’t know they have it until it’s too late.
Testing should happen before any high-risk medication is given. But here’s the catch: if you’ve just had a hemolytic episode, your enzyme levels look normal for up to 72 hours because the damaged cells are gone and the new ones haven’t matured yet. So you need to wait at least three months after a crisis to test accurately.
There are two main tests:
- Fluorescent spot test-Quick, cheap, and available in most clinics. Results in 15 minutes. Used widely in malaria-endemic countries.
- Quantitative spectrophotometric assay-The gold standard. Measures exact enzyme activity. Deficiency is defined as less than 10% of normal (under 1.7 U/g Hb).
New technology is changing the game. In January 2024, the FDA approved the first point-of-care quantitative test-the STANDARD G6PD Test System. It gives lab-grade results in 8 minutes. That’s huge for emergency rooms and clinics without labs.
And here’s another myth busted: women can have hemolytic crises too. Because of X-chromosome inactivation, up to 15% of female carriers have low enough enzyme levels to be at risk. It’s not just a "man’s disease."
Why This Isn’t Just About Drugs
It’s not just medications. Fava beans (broad beans) can trigger hemolysis in some people-especially those with Mediterranean variants. Infections like pneumonia or hepatitis can also cause oxidative stress. Even some herbal supplements and naphthalene (mothballs) are dangerous.
That’s why education matters. A study from the NIH found that 92% of patients who received full trigger avoidance education had no hemolytic episodes over five years. Only 38% of those who got standard care stayed safe.
Health systems are starting to catch up. At UCSF, an electronic health record system now flags 87 high-risk drugs automatically if G6PD status is known. In a 12-month pilot, inappropriate prescribing dropped by 89%.

What You Can Do
If you’ve never been tested:
- Ask your doctor for a G6PD test-especially if you’re of African, Mediterranean, Middle Eastern, or Southeast Asian descent.
- Get tested before any surgery, chemotherapy, or malaria treatment.
- Keep a card or app note listing your G6PD status and the drugs to avoid.
- Wear a medical alert bracelet if you’ve had a hemolytic episode.
- Teach your family. This is inherited. Your children may carry it too.
If you’ve been diagnosed:
- Keep a list of safe and unsafe medications. Update it every time you see a new doctor.
- Don’t assume your doctor knows. Bring your own list.
- Be cautious with over-the-counter drugs. Many contain sulfonamides or aspirin.
- Never take primaquine without proof of testing.
The Bigger Picture
There are 127 countries where G6PD deficiency affects more than 5% of the population. That’s 3.2 billion people. The WHO recommends universal newborn screening in these areas. Only 18 of 47 African countries have done it. In the U.S., only 12 states require newborn G6PD testing-even though 1 in 10 African American males has it.
The tools exist. The science is clear. The cost of testing is low-under $5 in many places. The cost of not testing? Blood transfusions, ICU stays, and sometimes death.
By 2035, experts believe preventable deaths from G6PD deficiency could be nearly eliminated in places with strong healthcare systems. But that won’t happen unless patients speak up and doctors listen.
Can I take acetaminophen if I have G6PD deficiency?
Yes. Acetaminophen (paracetamol) is considered safe for people with G6PD deficiency at standard doses. It doesn’t cause oxidative stress on red blood cells. Avoid aspirin, ibuprofen, and other NSAIDs unless your doctor confirms your deficiency is very mild (Class IV), as these can trigger hemolysis in some cases.
Is G6PD deficiency only a problem for men?
No. While G6PD deficiency is X-linked and more common in men, women can be affected too. Due to X-chromosome inactivation, up to 15% of female carriers have enzyme levels low enough to experience hemolysis. This is often overlooked, leading to dangerous misdiagnoses. Always test women with family history or from high-prevalence regions.
Can I get tested after a hemolytic episode?
Not right away. After a hemolytic crisis, your body replaces damaged red blood cells with new ones that have normal enzyme levels. This can make test results falsely normal. Wait at least three months after the episode for an accurate reading. If you’re in a hurry, genetic testing can identify the mutation regardless of recent hemolysis.
Are there any new treatments for G6PD deficiency?
Currently, there’s no cure, but prevention is highly effective. Research is advancing: N-acetylcysteine (NAC) has shown promise in lab studies to protect red blood cells during oxidative stress. Phase I trials for recombinant human G6PD enzyme replacement therapy are scheduled to begin in late 2024. For now, avoiding triggers remains the only proven method.
What should I do if I accidentally take a dangerous medication?
Stop the medication immediately. Seek medical help. Watch for symptoms: dark urine, extreme fatigue, yellowing skin, rapid heartbeat, or shortness of breath. Blood tests will check your hemoglobin and reticulocyte count. Treatment may include fluids, oxygen, and possibly a blood transfusion. The sooner you act, the better your outcome.






Matt Davies
December 21, 2025 AT 02:45