Every year, millions of people take herbal supplements thinking they’re doing something good for their health. But what if those same products are quietly damaging your liver? It’s not a myth. Herbal and supplement liver toxicity is real, growing, and often overlooked - even by doctors.
The liver is your body’s main detox hub. It filters everything you swallow, from coffee to vitamins to that trendy turmeric capsule you saw on TikTok. But when you overload it with unregulated botanicals, it doesn’t just work harder - it can start to shut down. And you might not notice until it’s too late.
These Six Supplements Are the Most Dangerous for Your Liver
According to a 2024 study in JAMA Network Open, six herbal and supplement ingredients have been repeatedly linked to serious liver injury in the U.S.:
- Turmeric or curcumin - Often marketed as an anti-inflammatory, high-dose turmeric supplements have caused hospitalizations. One study found that people taking more than 1,000 mg daily for months had spikes in liver enzymes. Some products also contained lead - 30% of tested turmeric supplements exceeded California’s safety limits.
- Green tea extract - The antioxidant EGCG sounds healthy, but concentrated doses (like in weight-loss pills) can be toxic. The liver struggles to process large amounts. In fact, 25% of green tea extract products exceeded the recommended daily limit for EGCG.
- Garcinia cambogia - Popular for weight loss, this extract has been tied to acute hepatitis. It’s often sold as a “natural” fat burner, but the liver can’t handle the chemical load.
- Black cohosh - Used for menopause symptoms, this herb has caused liver failure in multiple documented cases. The FDA has issued warnings, yet it’s still widely available.
- Red yeast rice - Marketed as a “natural statin,” it contains monacolin K, the same compound as the prescription drug lovastatin. But without medical supervision, it can cause rhabdomyolysis and liver damage.
- Ashwagandha - This adaptogen is promoted for stress and sleep, but recent data shows it’s increasingly linked to liver inflammation, especially in people taking it long-term or in high doses.
These aren’t rare cases. Between 2007 and 2015, herbal supplements caused over 21% of all drug-induced acute liver failure cases in the U.S. That’s more than some prescription drugs.
Why Your Liver Can’t Handle These Products
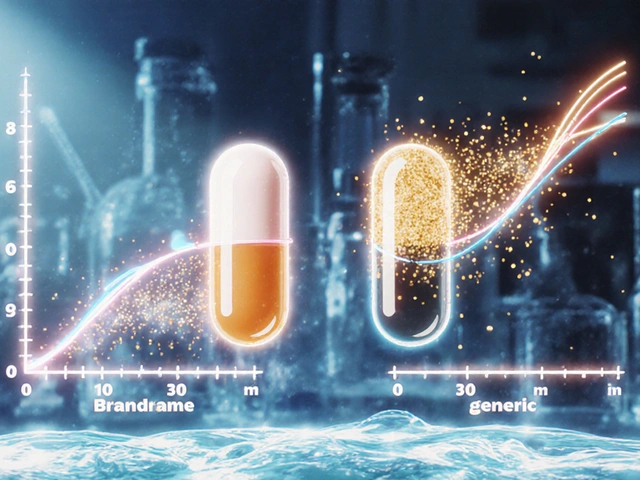
Your liver breaks down everything you take. But unlike pharmaceuticals, herbal supplements don’t go through safety testing before hitting store shelves. There’s no requirement for clinical trials, no mandatory dosing limits, and no monitoring for side effects.
Here’s what’s happening behind the scenes:
- Unknown ingredients - Up to 60% of tested supplements don’t match their labels. One product labeled as “pure ashwagandha” was found to contain undisclosed pharmaceuticals.
- Contaminants - Heavy metals like lead (found in 18% of products), mercury (12%), and arsenic (9%) show up in herbal products. Pesticides were detected in 23% of tested samples.
- Hidden drugs - Sexual enhancement supplements often contain sildenafil (Viagra) without listing it. Pain relievers have been found to include NSAIDs or even corticosteroids.
And the timing? It’s not consistent. The same herb harvested in spring vs. fall can have wildly different chemical levels. Roots vs. leaves? Different potency. Soil quality? Affects metal absorption. No two batches are the same - and your body doesn’t know how to adjust.
How to Tell If Your Liver Is in Trouble
Most people don’t feel liver damage until it’s advanced. But there are warning signs:
- Fatigue - 87% of cases report extreme tiredness that doesn’t improve with rest.
- Abdominal pain - Especially in the upper right side, under your ribs.
- Nausea or vomiting - Not just from food poisoning, but persistent.
- Dark urine - Like cola or tea. This is a classic sign of bilirubin buildup.
- Yellow skin or eyes - Jaundice. A late-stage symptom, but unmistakable.
These symptoms often appear weeks or months after starting a supplement. People think, “I’ve been taking this for months - it must be fine.” But liver damage builds silently.
Who’s Most at Risk?
It’s not just “people who take too many pills.” Anyone can be affected. But some are more vulnerable:
- People over 50 - Liver function declines with age.
- Those with pre-existing liver conditions - Fatty liver, hepatitis, or even past alcohol use increases risk.
- People on multiple medications - Supplements can interact with blood thinners, diabetes drugs, or antidepressants.
- Women - Some studies suggest women may be more susceptible to certain herbal liver toxins.
- Genetic outliers - Early research points to a gene variant (HLA-B*35:01) that makes some people far more likely to have a toxic reaction.
Think of it like a food allergy. One person eats peanuts and feels fine. Another goes into anaphylaxis from a tiny trace. With supplements, it’s the same - your body’s reaction isn’t about dose alone. It’s about your unique biology.
The Regulatory Gap
The FDA doesn’t approve supplements before they’re sold. Unlike prescription drugs, manufacturers don’t need to prove safety, effectiveness, or purity. They can sell anything - as long as they don’t claim it treats disease.
That’s why you’ll see products labeled “for wellness” or “supports immune function.” It’s a loophole. And it’s why so many products contain hidden drugs or heavy metals. There’s no routine testing. No recalls unless someone dies.
Dr. Robert S. Brown of Weill Cornell Medicine put it bluntly: “The liver damage caused by supplements is identical to the damage caused by pharmaceuticals.” But unlike drugs, supplements have no safety net.

What You Should Do
Don’t stop taking supplements blindly. But do this:
- Stop all herbal supplements if you have unexplained fatigue, nausea, or dark urine. Go to your doctor. Tell them exactly what you’re taking - brand names, doses, how long.
- Ask for liver enzyme tests. ALT and AST levels are simple blood tests. If they’re elevated, stop everything and retest in 4-6 weeks. Often, liver function returns to normal after stopping the supplement.
- Don’t trust labels. Look for third-party testing seals: USP, NSF, or ConsumerLab. These don’t guarantee safety, but they check for contamination.
- Check the LiverTox database. Run by the NIH, it lists every supplement linked to liver injury. Search by name - it’s free and updated regularly.
- Ask your doctor before starting anything. Especially if you’re on medication or have any liver history.
And if you’re taking supplements because of social media trends - pause. TikTok influencers aren’t trained in hepatology. A viral “liver cleanse” with 12 herbal ingredients? That’s a recipe for disaster.
What’s Being Done?
The American College of Gastroenterology now recommends doctors routinely ask patients about supplement use during liver evaluations. Some hospitals are starting to screen for herbal toxins in cases of unexplained liver injury.
But real change needs regulation. Until supplements are held to the same standards as drugs, the risk remains. Until then, your best defense is awareness.
Can turmeric really damage your liver?
Yes. While turmeric in food is safe, concentrated supplements - especially high-dose or long-term - have caused liver injury in multiple documented cases. Some products also contain lead, which adds to the risk. The JAMA Network Open study identified turmeric as one of the top six supplements linked to liver damage.
Are all herbal supplements dangerous?
No. Many herbs are safe when used appropriately. But the problem isn’t the herbs themselves - it’s the lack of regulation. Products can be contaminated, mislabeled, or contain hidden drugs. Without knowing what’s really in them, you can’t know if they’re safe.
How long does it take for supplements to damage the liver?
It varies. Some people develop liver injury after a few weeks. Others take months or even years. The damage builds slowly and often has no symptoms at first. That’s why it’s so dangerous - you won’t feel it until it’s serious.
Can liver damage from supplements be reversed?
In many cases, yes - if caught early. Stopping the supplement and avoiding alcohol or other liver stressors can allow the liver to heal. But if damage is severe or prolonged, scarring (fibrosis) can become permanent. Early detection through blood tests is critical.
Should I stop taking supplements if I’m healthy?
Not necessarily - but be cautious. If you’re taking supplements for vague reasons like “energy” or “detox,” there’s little evidence they help. If you’re taking them for a specific condition, talk to your doctor. For most people, a balanced diet provides everything the body needs.