Methotrexate-NSAID Interaction Risk Calculator
Assess Your Risk
Risk Assessment Results
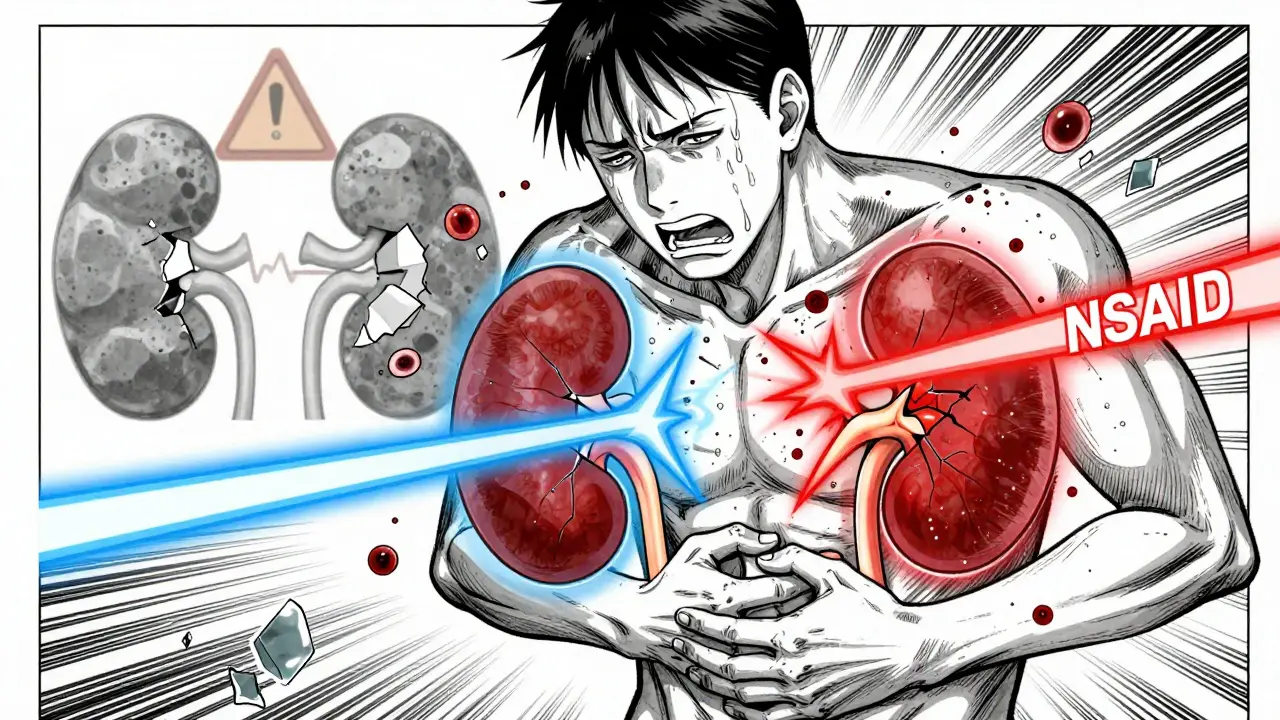
When you're managing rheumatoid arthritis with methotrexate, pain relief shouldn’t come at the cost of your kidneys. Yet, millions of patients take NSAIDs like ibuprofen or naproxen alongside methotrexate without realizing how dangerous this combo can be. It’s not just about stomach upset or high blood pressure - this interaction can spike methotrexate levels by up to 50%, leading to life-threatening kidney damage, bone marrow suppression, and even death. The science is clear. The risks are real. And too many patients are being caught off guard.
Why Methotrexate and NSAIDs Don’t Mix
Methotrexate isn’t just a typical drug. At low doses (5-25 mg weekly), it’s used for autoimmune diseases like rheumatoid arthritis. At high doses (over 150 mg), it’s a cancer drug. Either way, your kidneys are the main route out for methotrexate. About 80% of it leaves your body through urine, mostly by active transport in the kidney tubules. That’s why anything that messes with kidney function - like NSAIDs - can cause methotrexate to build up dangerously.
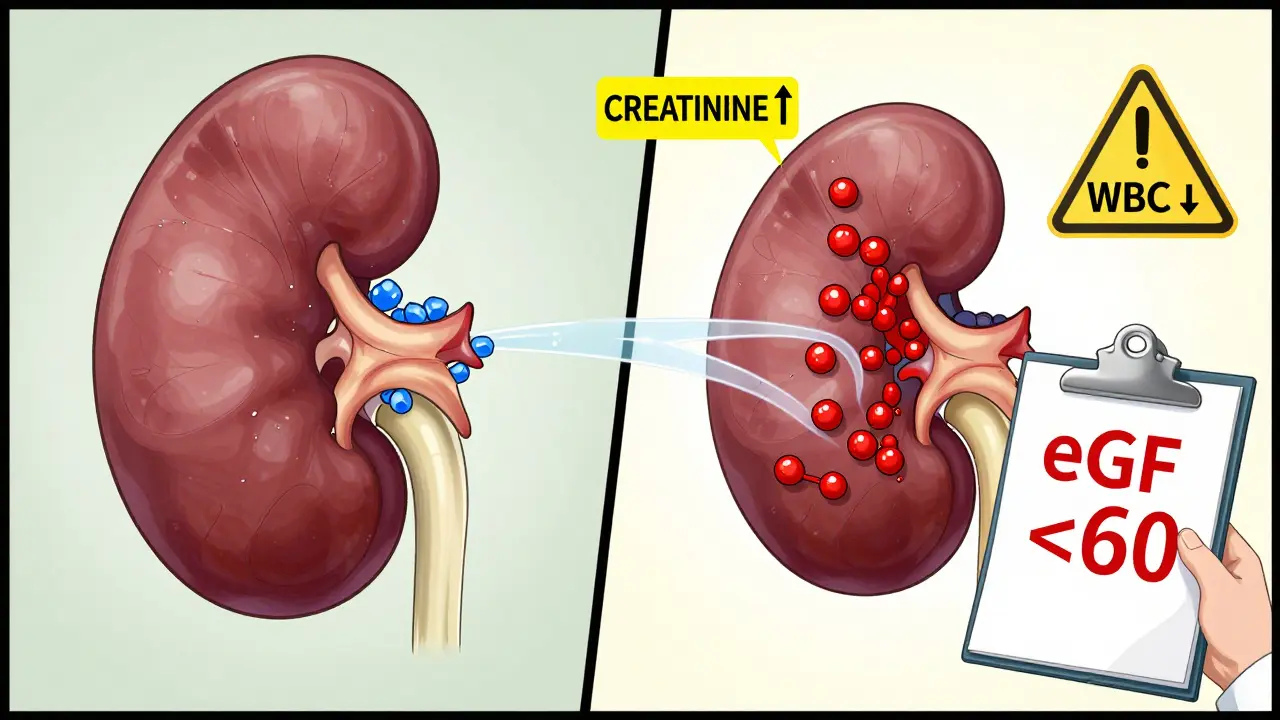
NSAIDs work by blocking prostaglandins, chemicals that help keep blood flowing to your kidneys. When those prostaglandins drop, your kidneys get less blood. That means less filtration. Less clearance. And that’s exactly what happens when you take an NSAID with methotrexate: methotrexate sticks around longer. Studies show renal clearance drops by 25-40%. In some cases, serum methotrexate levels rise by 30-50%. That’s not a small bump. That’s a red alert.
It’s not just about blood flow. NSAIDs also compete with methotrexate for the same transporters in the kidney tubules. Think of it like two cars trying to get through a single toll booth at the same time. One (methotrexate) gets stuck. The other (NSAID) goes through fine - but the backup causes chaos. This competitive inhibition is proven in lab studies and confirmed in real patients.
High-Dose vs. Low-Dose: The Risk Difference
Not all methotrexate is the same. The risk changes dramatically depending on the dose.
For cancer patients getting high-dose methotrexate (500 mg/m² or more), combining it with NSAIDs is a known killer. A 2022 meta-analysis found the risk of severe toxicity - like acute kidney injury or fatal bone marrow failure - jumps by 4.7 times. Between 2018 and 2022, the FDA recorded three deaths directly linked to this combo in oncology settings. That’s why the National Comprehensive Cancer Network (NCCN) says: if you’re giving high-dose methotrexate, avoid NSAIDs entirely. If you absolutely must, monitor methotrexate levels at 24, 48, and 72 hours after administration.
For rheumatoid arthritis patients on low-dose methotrexate (≤25 mg weekly), the picture is more complex. Some large studies, like the 2019 Annals of the Rheumatic Diseases trial with over 4,000 patients, found no significant rise in serious side effects when NSAIDs were added - but only if kidney function was normal. That’s the key. When patients already had reduced kidney function (eGFR below 60), the risk of hospitalization for kidney injury jumped 3.5 times. A 2021 review in Rheumatology found a 3.2-fold increase in adverse events in this group.
So it’s not that NSAIDs are safe with low-dose methotrexate. It’s that the danger is hidden - unless you’re checking kidney numbers regularly.
Which NSAIDs Are the Worst?
Not all NSAIDs are created equal when it comes to methotrexate interactions.
Ketorolac is the worst offender. It’s a potent, short-acting NSAID often used in hospitals for severe pain. Studies show it can raise methotrexate levels by up to 50%. That’s why it’s banned in many outpatient settings for patients on methotrexate.
Ibuprofen and naproxen are next in line. They typically increase methotrexate levels by 25-30%. That’s still dangerous, especially if taken daily or if the patient is older or dehydrated.
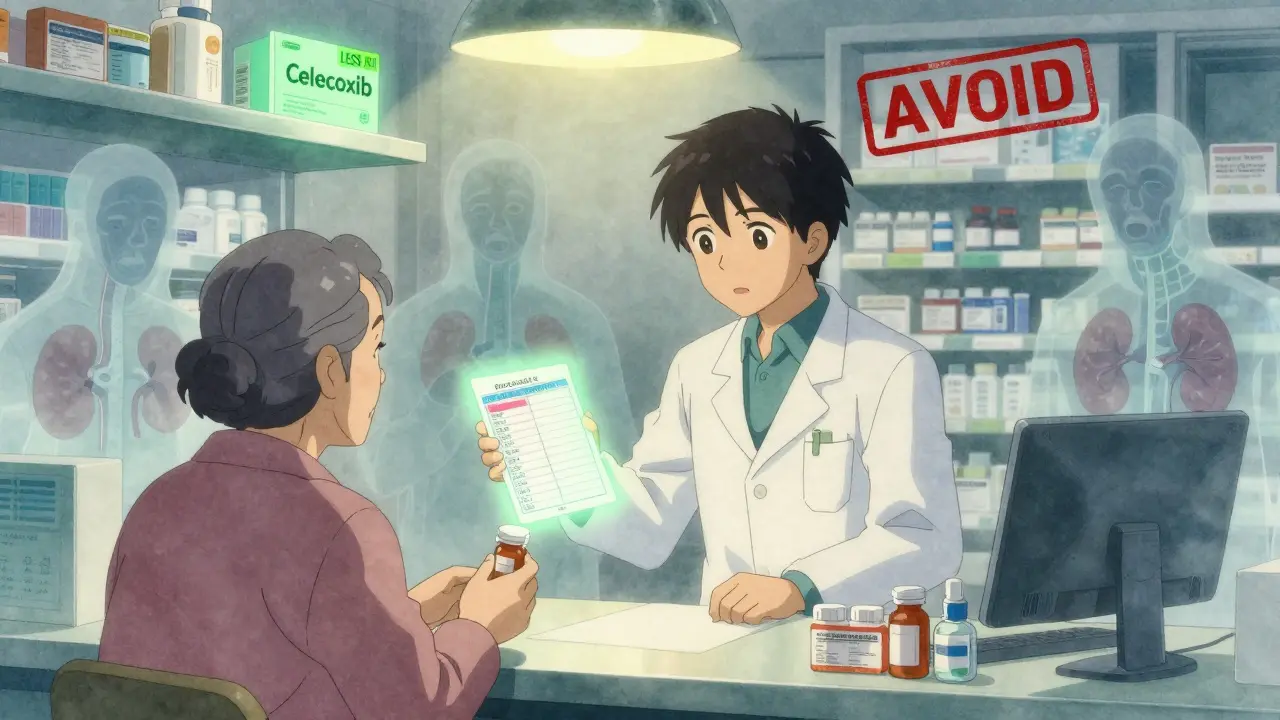
Diclofenac is also risky, though slightly less so than ibuprofen. Celecoxib, a COX-2 selective NSAID, shows the lowest interaction potential - around 10-15% increase in methotrexate levels. That’s why some rheumatologists consider celecoxib a safer option for patients who absolutely need an NSAID and have normal kidney function.
But here’s the catch: even celecoxib isn’t risk-free. The difference is small, and it doesn’t eliminate the danger. The only truly safe NSAID for methotrexate users? None. That’s why guidelines now say: avoid them if possible.
Who’s Most at Risk?
Age and kidney health are the biggest red flags.
Patients over 65 are 2.8 times more likely to die from a methotrexate-NSAID interaction, according to EULAR’s analysis of European registries. Why? Kidneys naturally decline with age. Liver function drops. Hydration often worsens. And many older patients are on multiple meds that add to the burden.
People with existing kidney disease - even mild - are at extreme risk. An eGFR below 60 mL/min/1.73m² is a hard stop for NSAIDs in most guidelines. Yet, a 2022 analysis by the Institute for Safe Medication Practices found that 78% of serious interaction cases happened in patients who hadn’t had a kidney test in the last 30 days.
Genetics also play a role. A 2023 study from the Methotrexate Genetics Consortium found that about 15% of Caucasians carry a gene variant called SLC19A1 80G>A. These patients absorb methotrexate more easily and clear it much slower - especially when NSAIDs are added. Their methotrexate levels can spike 40% higher than non-carriers. This isn’t theoretical. It’s measurable. And it’s not routinely tested.
What Happens When Things Go Wrong?
The signs aren’t always obvious. That’s why this interaction is so deadly.
Early symptoms - fatigue, nausea, mouth sores, loss of appetite - are easy to dismiss as “just getting older” or “the flu.” But they’re often the first warning signs of methotrexate toxicity. Blood tests reveal the real story: rising creatinine (kidney damage), dropping white blood cell counts (bone marrow suppression), and sometimes liver enzyme spikes.
One Reddit user, ‘RAWarrior2020,’ described taking naproxen for knee pain. Within three days, his white blood cell count crashed to 1.8 × 10⁹/L (normal is 4-11). He ended up in the hospital needing leucovorin - a rescue drug that reverses methotrexate’s effects. It took two weeks to recover.
Another patient, ‘MTXandMe,’ has taken methotrexate with occasional ibuprofen for eight years - but only because her doctor checks her kidney and blood counts every four weeks. That’s the difference: monitoring.
A 2022 Arthritis Foundation survey showed that 41% of patients who took NSAIDs with methotrexate without regular testing had at least one adverse event. Only 9% did when monitoring was in place.
How to Stay Safe
There’s no magic fix. But there are clear, proven steps to reduce risk.
- Avoid NSAIDs if your eGFR is below 60. That’s non-negotiable.
- Use the lowest dose of NSAID for the shortest time. No daily use. No long-term use.
- Space out doses. Take methotrexate in the morning, NSAID in the evening - or vice versa - to reduce peak concentration overlap.
- Test before and after. Get a creatinine and CBC 48-72 hours after starting an NSAID. If creatinine rises more than 25%, stop the NSAID.
- Consider alternatives. Acetaminophen (up to 3 g/day) is safer. Low-dose opioids for short-term flare-ups. Or better yet - optimize your DMARDs to reduce pain at the source.
- Ask your pharmacist. A 2023 study showed pharmacist-led medication reviews cut interaction rates by 63% in Medicare patients. They catch what doctors miss.
For high-dose methotrexate patients, monitoring is mandatory. Blood levels at 24, 48, and 72 hours. Hydration. Urine output tracking. No exceptions.
The Bottom Line
Methotrexate and NSAIDs aren’t just a bad combo - they’re a ticking time bomb for people with kidney vulnerability. The data doesn’t lie. The deaths aren’t rare. The warnings are out there.
But the biggest problem isn’t the science. It’s the silence. Too many patients are prescribed NSAIDs without being told the risks. Too many doctors assume “low-dose” means “safe.” It doesn’t. Not without monitoring.
If you’re on methotrexate, don’t take an NSAID without checking your kidney function first. If you’re a doctor, don’t prescribe one without asking if your patient’s last creatinine test was within the last 30 days. And if you’re a pharmacist - speak up. You’re often the last line of defense.
This isn’t about fear. It’s about awareness. And in medicine, awareness saves lives.
Can I take ibuprofen with methotrexate if my kidneys are fine?
It’s not recommended, but some doctors allow occasional, low-dose ibuprofen (200-400 mg) in patients with normal kidney function (eGFR >60) and no other risk factors. Even then, it should be used sparingly - no more than a few days at a time - and only after checking creatinine and blood counts 48-72 hours after starting. Never use it daily. Always talk to your rheumatologist first.
What are the early signs of methotrexate toxicity from NSAIDs?
Early signs include extreme fatigue, nausea, vomiting, mouth sores, and unexplained bruising or bleeding. These often appear within 2-5 days of starting the NSAID. Blood tests will show rising creatinine (kidney stress) and falling white blood cell or platelet counts. If you feel unusually tired or get mouth ulcers after starting an NSAID, stop it and get tested immediately.
Is celecoxib safer than other NSAIDs with methotrexate?
Yes, celecoxib has the lowest interaction potential, raising methotrexate levels by only 10-15% compared to 25-50% with other NSAIDs. This is because it targets COX-2, which has less impact on kidney blood flow. But it’s not safe - just less risky. It still carries a warning in the FDA label. Avoid it if your eGFR is below 60 or if you’re over 65. Never assume it’s harmless.
Can I take acetaminophen instead of NSAIDs with methotrexate?
Yes, acetaminophen (up to 3,000 mg per day) is the preferred pain reliever for people on methotrexate. It doesn’t affect kidney blood flow or methotrexate clearance. It’s not anti-inflammatory like NSAIDs, so it won’t reduce joint swelling - but it’s much safer for pain relief. Always check with your doctor if you have liver disease, as acetaminophen can be toxic at high doses in that case.
How often should I get my kidney function checked if I’m on methotrexate?
If you’re on methotrexate alone, check creatinine and CBC every 4-8 weeks. If you start an NSAID - even for a few days - get tested 48-72 hours after the first dose. If you’re over 65, have diabetes, high blood pressure, or any kidney disease, test every 2-4 weeks regardless of NSAID use. Routine testing catches problems before symptoms appear.
Are there any new tests to monitor methotrexate levels in real time?
Yes, point-of-care methotrexate level tests are currently in phase 3 clinical trials (NCT05123456). These devices could give results in under an hour using a finger-prick blood sample. If approved, they’ll be especially useful for patients on high-dose methotrexate or those needing NSAIDs for pain. But they’re not available yet. Until then, standard blood tests are your best tool.





Andrew Smirnykh
January 23, 2026 AT 10:04