When your hip starts to ache with every step, it’s not just discomfort-it’s a signal that something deeper is wrong. Osteoarthritis of the hip isn’t just "wear and tear." It’s a slow, painful breakdown of the cartilage that cushions your joint, leading to bone rubbing on bone, inflammation, and stiffness that makes walking, climbing stairs, or even getting out of bed a struggle. And if you’re carrying extra weight, you’re not just adding pounds-you’re adding pressure. Every extra pound puts three to six times more force on your hip joint with each step. That’s why weight loss isn’t just a nice-to-have for people with hip osteoarthritis-it’s one of the most powerful, evidence-backed tools you have to slow the damage and feel better.
Why Weight Loss Matters More Than You Think
Many people assume that because hip osteoarthritis affects the joint differently than knee OA, weight loss won’t help. But that’s a myth. While some early studies suggested hip OA didn’t respond much to weight loss, newer research paints a clearer picture. A 2024 study published in Nature followed 65-year-old adults with hip OA and obesity. Those who lost more than 10% of their body weight saw a 31% improvement in their quality of life related to hip function. Pain dropped. Stiffness eased. Walking became easier. And the bigger the weight loss, the better the results. This isn’t about looking a certain way. It’s about reducing the mechanical load on a joint that’s already struggling. Think of your hip like a car bearing. If the tires are worn and you keep driving with heavy cargo, the bearings wear out faster. Lose the extra weight, and the stress drops. That gives your body a chance to heal, or at least slow the damage.The Numbers Don’t Lie: How Much Weight Do You Really Need to Lose?
You’ve probably heard "lose 5% of your body weight" as a general rule for arthritis. That’s based mostly on knee OA data. But for the hip, the evidence suggests you need to aim higher. Studies show that losing 5% might help a little, but losing 7% to 10% is where you start seeing real, measurable improvements. In the Nature study, participants who lost over 10% saw the biggest gains across all measures: pain, mobility, stiffness, and even sports and daily activity scores. Another review in the Journal of Metabolic Health found that people who lost 10% or more had significantly better function than those who lost less than 5%. And here’s the kicker: losing 20% didn’t give you much more benefit than losing 10%. So there’s a sweet spot-10% is the target for meaningful, lasting relief. For someone weighing 200 pounds, that’s just 20 pounds. For someone at 250, it’s 25 pounds. It’s not about becoming thin. It’s about getting to a weight that takes the pressure off your hip.Why Hip OA Is Different from Knee OA (And What That Means for You)
Here’s where things get confusing. Some doctors still say weight loss doesn’t help hip OA. That’s because early studies were messy. One 2023 trial compared a very-low-calorie diet plus exercise to exercise alone in people with hip OA. At six months, there was no big difference in pain levels. But at 12 months? The group that lost weight had better pain scores, better function, and more overall improvement. That delay matters. Your body doesn’t fix joints overnight. The inflammation takes time to calm down. The cartilage doesn’t regenerate, but the surrounding muscles do. And when you lose weight, your body can start moving better-less pain, more movement, better circulation to the joint. It’s a snowball effect. Knee OA responds faster to weight loss because the knee bears direct, linear force with every step. The hip? It’s a ball-and-socket joint, more stable, more complex. So changes are subtler-but they’re still there. Don’t let outdated opinions discourage you. The latest data is clear: if you’re overweight and have hip OA, losing weight works.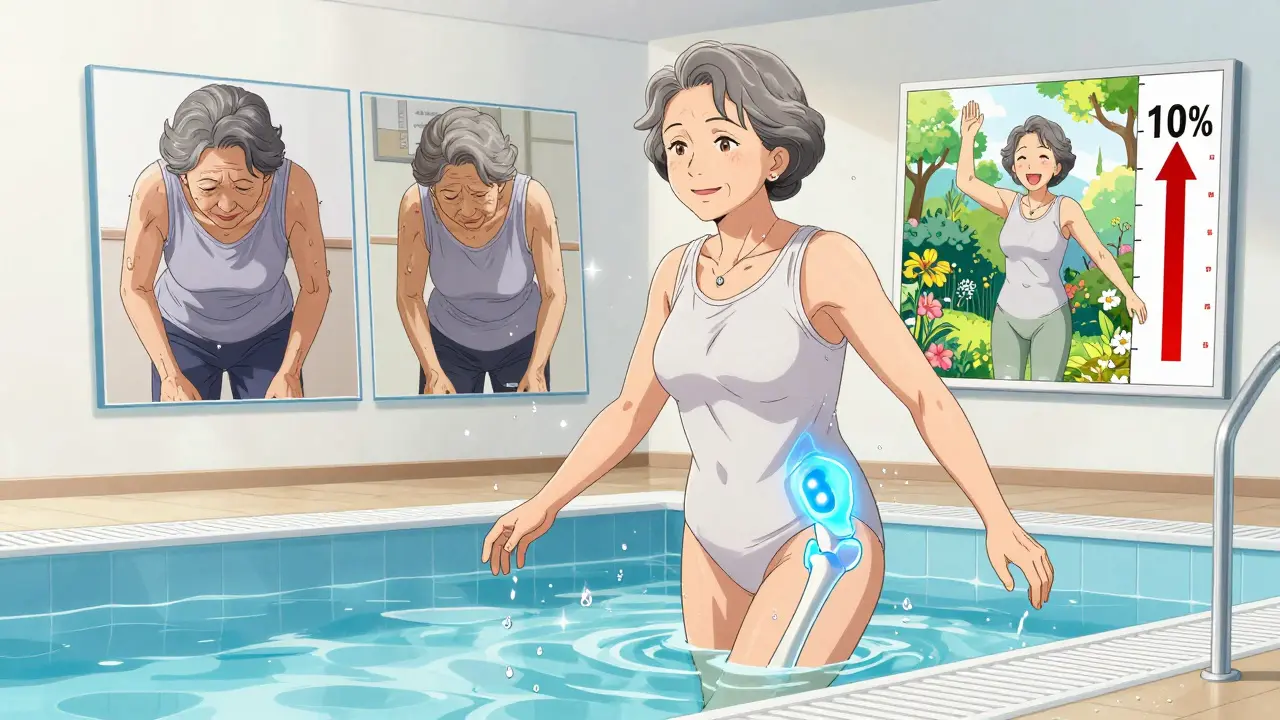
What Actually Works: Diet, Exercise, and Structure
Losing weight isn’t about going on a fad diet. It’s about building a sustainable plan. The Osteoarthritis Healthy Weight For Life (OAHWFL) program-originally designed for knee OA and now adapted for hip OA-shows how it’s done. It’s an 18-week program combining:- Low-carbohydrate, nutrient-dense eating
- Structured, low-impact exercise (like swimming, cycling, or tai chi)
- Weekly coaching and accountability
What to Avoid: The Pitfalls of Weight Loss with Hip OA
Not all weight loss strategies are created equal. Here’s what doesn’t work-and can even hurt you:- High-impact exercise like running or jumping: It’s too hard on the joint. Stick to swimming, elliptical, or seated cycling.
- Extreme diets that cut out all carbs or fat: They’re unsustainable and can lead to muscle loss, which makes joint support worse.
- Going it alone: People who try to lose weight without support are far less likely to succeed. Join a program, work with a dietitian, or find a buddy.
- Waiting until you’re in severe pain: The earlier you act, the more joint you preserve. Don’t wait until you can’t walk.
When Weight Loss Isn’t Enough: What Else Helps?
Weight loss is powerful-but it’s not magic. Combine it with these proven strategies:- Strength training: Focus on glutes, quads, and core. Strong muscles act like shock absorbers for your hip.
- Physical therapy: A PT can teach you safe movement patterns and stretches that reduce joint stress.
- Anti-inflammatory diet: Eat more omega-3s (salmon, walnuts), leafy greens, berries, and turmeric. Cut back on sugar and processed foods.
- Assistive devices: A cane used in the opposite hand can reduce hip pressure by up to 20%.
- Medications: If needed, acetaminophen or NSAIDs can help manage pain short-term. But they don’t fix the root cause.
Real People, Real Results
Maria, 62, was diagnosed with hip OA after years of chronic pain. She weighed 210 pounds and could barely walk to her mailbox. She joined a 16-week program that combined a low-carb meal plan with twice-weekly water aerobics. She lost 23 pounds-11% of her body weight. Within six months, she stopped using her cane. She started gardening again. She took a trip to visit her grandchildren without needing pain meds. James, 58, tried everything-shots, braces, physical therapy. Nothing stuck. He started tracking his food, swapped soda for sparkling water, and walked 20 minutes every day. He lost 18 pounds. His pain dropped from an 8/10 to a 3/10. He didn’t get surgery. He just got healthier. These aren’t rare cases. They’re the norm when people take consistent, smart action.The Bottom Line: Your Hip Can Still Have a Future
Hip osteoarthritis doesn’t have to mean surgery. It doesn’t have to mean giving up the things you love. Weight loss isn’t a cure-but it’s the most effective non-surgical tool we have to preserve your joint, reduce pain, and keep you moving. You don’t need to lose 50 pounds. You don’t need to run a marathon. You just need to lose enough-around 10% of your body weight-to take the pressure off your hip. Do it with a plan. Do it with support. Do it with patience. The science is clear. The results are real. And your next step? Start today. Not tomorrow. Not next month. Today.Can losing weight really help hip osteoarthritis, or is that just for knee pain?
Yes, weight loss helps hip osteoarthritis, but the effects are often slower and less dramatic than with knee OA. Recent studies, including a 2024 Nature trial, show that losing 10% or more of your body weight leads to significant improvements in pain, function, and quality of life. While some older studies suggested little benefit, newer, better-designed research confirms that reducing weight eases joint stress and improves symptoms.
How much weight should I aim to lose for hip OA relief?
Aim for 7% to 10% of your total body weight. Losing 5% may help a little, but studies show the biggest improvements come at 10% or more. For example, a person weighing 200 pounds would see major symptom relief after losing 20 pounds. Losing more than 10% (like 15-20%) doesn’t usually add much extra benefit, so 10% is the sweet spot.
What kind of diet works best for hip osteoarthritis and weight loss?
A balanced, low-carbohydrate, whole-food diet works best. Focus on lean proteins, vegetables, healthy fats (like avocado and olive oil), and fiber-rich foods. Avoid sugary drinks, refined carbs, and processed snacks. Programs like the Osteoarthritis Healthy Weight For Life (OAHWFL) have shown success using this approach. It’s not about starving-it’s about eating smarter to reduce inflammation and support joint health.
Is exercise safe if my hip hurts?
Yes-but only the right kind. High-impact activities like running or jumping can make hip pain worse. Stick to low-impact options: swimming, cycling, water aerobics, tai chi, or seated strength training. These build muscle around the hip without pounding the joint. Physical therapy can help you learn safe movement patterns. Movement is medicine, even when it hurts-just choose movements that protect your joint.
How long does it take to see results from weight loss for hip OA?
It takes time. Some people notice less stiffness or better mobility within 2-3 months. But the biggest improvements-like reduced pain and improved walking ability-often show up after 6 to 12 months. A 2023 study found no major pain difference at 6 months, but by 12 months, the weight-loss group had significantly better outcomes. Patience and consistency are key.
Should I consider weight-loss medications for hip OA?
Weight-loss medications like semaglutide or tirzepatide are FDA-approved for people with BMI over 30 (or over 27 with other health risks). They can help if lifestyle changes alone aren’t enough-but they’re not a first step. Doctors recommend trying diet, exercise, and behavioral support for at least 6 months before considering medication. These drugs work best when paired with healthy habits, not as a replacement.
Can I avoid hip replacement if I lose weight?
For many people, yes. While weight loss won’t reverse existing cartilage damage, it can slow progression and reduce symptoms enough to delay or even avoid surgery. Studies show that people who lose weight and strengthen their muscles around the hip are less likely to need a hip replacement in the next 5-10 years. It’s not guaranteed, but it’s one of the best ways to protect your joint long-term.




Payton Daily
December 28, 2025 AT 03:10