When your skin breaks out in thick, scaly patches and your fingers swell like sausages at the same time, it’s not just bad luck-it’s a signal. Psoriatic arthritis isn’t just psoriasis plus joint pain. It’s a single disease that attacks both your skin and your joints at once, driven by the same faulty immune response. About 30% of people with psoriasis will develop it. And if you’re one of them, understanding how these two symptoms connect isn’t just helpful-it’s critical to stopping permanent damage.
How Skin and Joints Are Connected in Psoriatic Arthritis
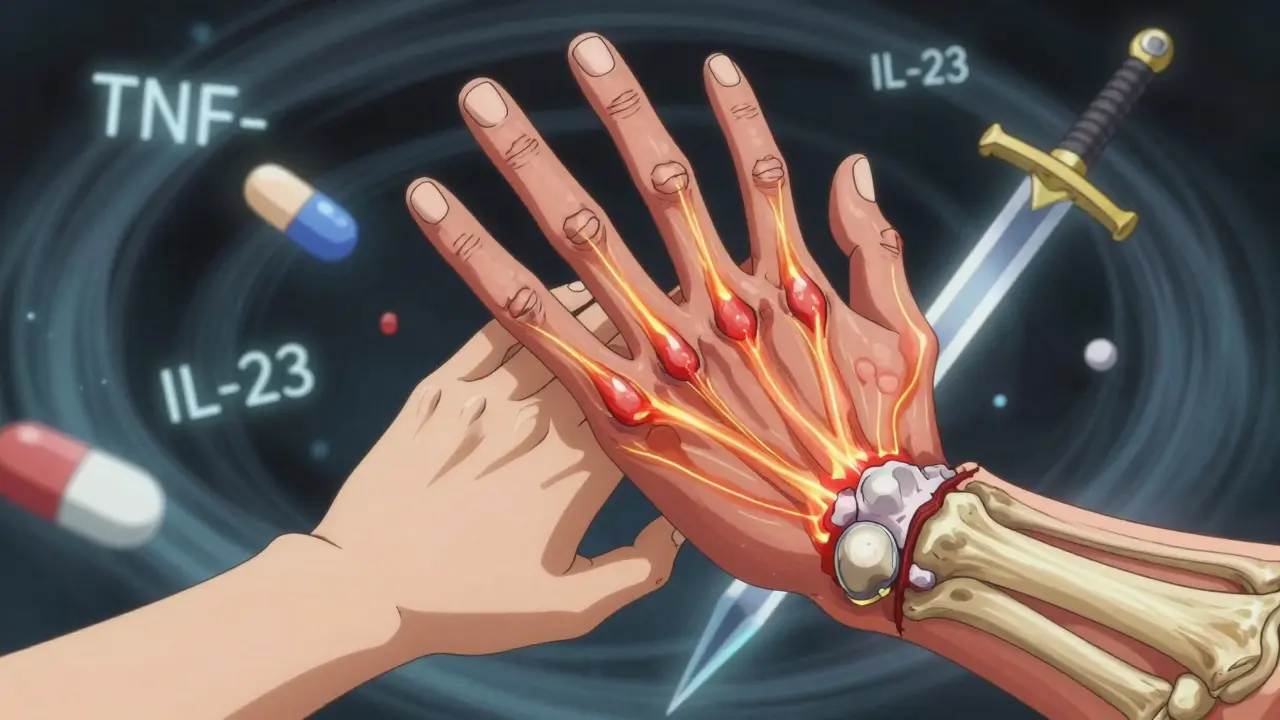
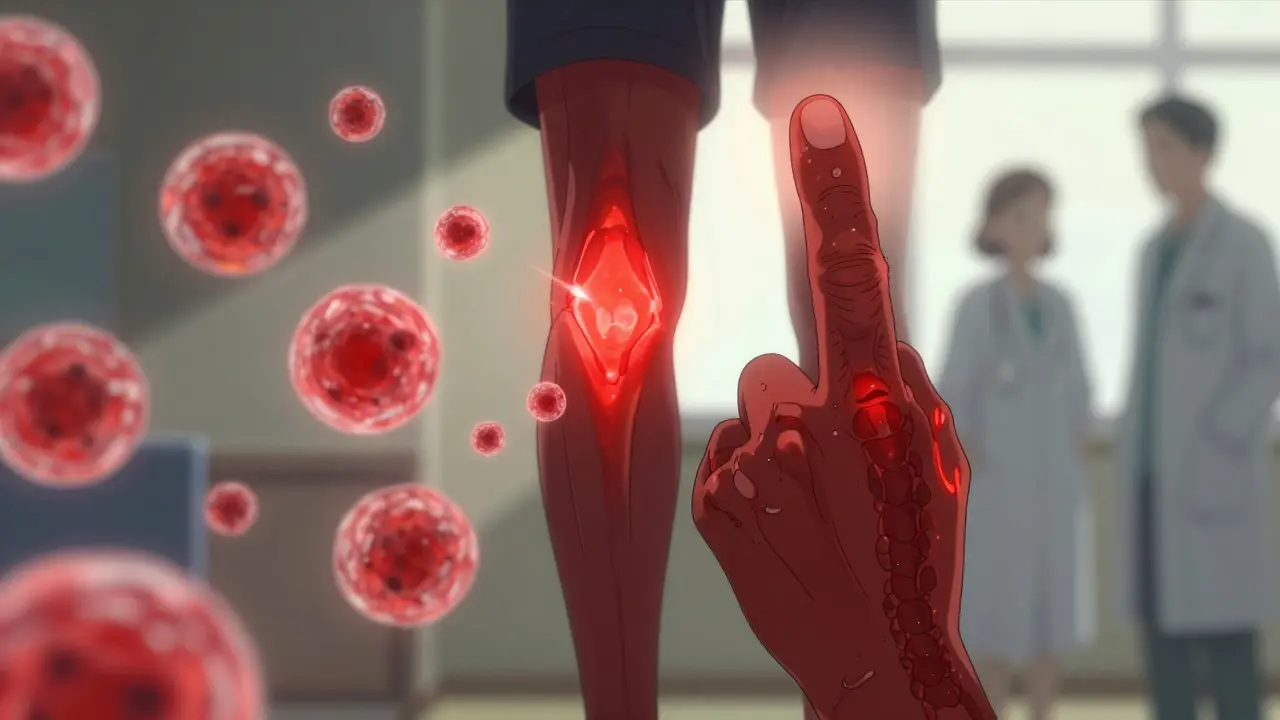
The link between psoriasis and psoriatic arthritis isn’t random. Both come from the same root: your immune system goes rogue. Instead of protecting you, it starts attacking healthy cells in your skin and the places where tendons and ligaments meet bone-called entheses. This is why you often see red, flaky plaques on your elbows or knees, and hours of stiff, achy joints in the same areas.
Unlike rheumatoid arthritis, which usually hits joints symmetrically (both wrists, both knees), psoriatic arthritis often strikes unevenly. You might have swelling in your right index finger but not the left. Or your left knee aches while your right knee feels fine. About 70% of cases show this pattern. And it’s not just the big joints. The tiny joints closest to your fingernails? Those are hit in 80% of cases. That’s why nail changes-pitting, ridges, or nails lifting off the nail bed-are such a big clue. If you have psoriasis and your nails look like they’ve been chewed up, don’t ignore it.
Another telltale sign is dactylitis. That’s when an entire finger or toe swells up like a sausage. It happens in 40-50% of people with psoriatic arthritis. It’s not just pain. It’s a whole digit that’s warm, tight, and hard to move. And enthesitis? That’s inflammation where tendons anchor into bone. It’s what causes heel pain that feels like walking on broken glass, or pain in the bottom of your foot from plantar fasciitis that won’t go away. These aren’t side effects-they’re core features of the disease.
Recognizing the Five Types of Psoriatic Arthritis
Not everyone with psoriatic arthritis has the same pattern. Doctors classify it into five types, and knowing which one you have helps guide treatment.
- Asymmetric oligoarthritis (70% of cases): Affects fewer than five joints, often in different areas on each side of the body. This is the most common form and often starts mild.
- Symmetric polyarthritis (25%): Mimics rheumatoid arthritis by affecting matching joints on both sides. But unlike RA, it usually comes with skin or nail changes.
- Distal interphalangeal predominant (5%): Hits the joints right under your fingernails. Often paired with severe nail damage. Easy to miss-it looks like just a bad nail.
- Spondylitis (5-20%): Involves your spine. You’ll feel stiffness in your lower back or neck, especially in the morning. It can feel like ankylosing spondylitis, but usually less severe.
- Arthritis mutilans (less than 5%): The rarest and most destructive. Causes bones to dissolve, leading to shortened, deformed fingers or toes. Often seen in untreated cases.
Most people start with asymmetric or distal forms. But if left unchecked, it can shift into more aggressive patterns. That’s why early recognition matters.
Why Diagnosis Takes So Long (and How to Speed It Up)
On average, people wait 2.3 years before getting the right diagnosis. Why? Because doctors often treat the skin and joints separately. A dermatologist sees your plaques. A rheumatologist sees your swollen knee. Neither connects the dots.
Here’s the problem: there’s no blood test that confirms psoriatic arthritis. Unlike rheumatoid arthritis, where the rheumatoid factor shows up in 70-80% of cases, 90% of psoriatic arthritis patients test negative. No CRP? No ESR spike? Doesn’t mean it’s not there. Diagnosis relies on clinical signs: skin lesions, nail changes, dactylitis, enthesitis, and asymmetric joint swelling.
That’s why seeing both a dermatologist and a rheumatologist together cuts diagnosis time in half. In fact, 45% of psoriatic arthritis cases are first spotted by dermatologists-so if you have psoriasis and new joint pain, don’t wait. Ask for a referral. If your doctor says, “It’s probably just aging,” push back. Early treatment within 12 weeks of joint symptoms can prevent irreversible damage in 75% of cases.
Treatment Options: From Creams to Biologics
Treatment has changed dramatically since the 2000s. Back then, options were limited to NSAIDs and methotrexate. Today, we have drugs that target the exact pathways causing inflammation in both skin and joints.
Topical treatments (creams, ointments) help with skin plaques but won’t touch joint pain. They’re useful for mild cases but not enough alone.
DMARDs like methotrexate or sulfasalazine slow disease progression. They’re often the first step if you have moderate joint involvement. But they take weeks to work, and about half of patients don’t respond well enough.
Biologics are the game-changers. These are injectable or IV drugs that block specific immune signals-like TNF-alpha, IL-17, or IL-23-that drive both psoriasis and arthritis. Examples include:
- Adalimumab (Humira) and Etanercept (Enbrel): TNF inhibitors. First-line biologics for many.
- Ustekinumab (Stelara): Blocks IL-12 and IL-23. Works well for both skin and joint symptoms.
- Guselkumab (Tremfya): Targets IL-23 specifically. Studies show 80% of users see 75% skin clearance and major joint improvement.
- Deucravacitinib (Sotyktu): The first oral TYK2 inhibitor approved in 2022. A pill that works as well as injections for many patients.
Most biologics reduce joint swelling by 50-80% within 3-6 months. Skin clears in as little as 4 weeks. But they’re expensive. Out-of-pocket costs for biologics average over $500 a month. Insurance approvals can take over two weeks. Talk to your doctor about patient assistance programs-most drugmakers offer them.
What Doesn’t Work (and What Might Surprise You)
Not all treatments help both skin and joints. Steroid injections into joints can relieve pain temporarily but don’t stop disease progression. And corticosteroid creams? Great for skin, useless for joints.
Some people try supplements like omega-3s or turmeric. They might help with general inflammation, but there’s no solid evidence they control psoriatic arthritis. Don’t skip prescribed meds for these.
Here’s a surprise: stress doesn’t cause psoriatic arthritis, but it’s the #1 trigger for flares. Anxiety, poor sleep, even a bad breakup can spark a flare-up. Managing stress isn’t optional-it’s part of treatment. Meditation, walking, therapy-these aren’t “nice to have.” They’re medicine.
Lifestyle Matters More Than You Think
Weight matters. Every extra pound puts more stress on your joints. Losing just 5-10% of body weight can cut joint pain in half. And it reduces inflammation system-wide.
Exercise isn’t just for fitness. Gentle movement-swimming, cycling, yoga-keeps joints flexible and prevents stiffness. Physical therapy is often overlooked but can teach you how to move without hurting yourself. A 2023 study showed patients who did 30 minutes of daily movement had 40% fewer flares.
Diet? No magic food, but cutting out processed sugar, refined carbs, and excess alcohol helps. These fuels inflammation. Eat more vegetables, fatty fish, nuts. It won’t cure you-but it gives your body a better chance to respond to treatment.
What to Expect Long-Term
There’s no cure. But with modern treatment, most people live full lives. Life expectancy is nearly normal if you manage the disease. The big risk? Heart disease. People with psoriatic arthritis have a 1.5 times higher risk of heart attack or stroke. That’s why regular blood pressure and cholesterol checks are non-negotiable.
Flare-ups will come. You’ll have good months and bad ones. That’s normal. The goal isn’t to be pain-free every day-it’s to reach “minimal disease activity.” That means: no swollen joints, minimal skin plaques, low fatigue, and no new damage on scans. About 40-60% of patients hit that target with the right combo of meds and lifestyle changes.
The future is brighter. AI is now predicting who’ll develop psoriatic arthritis from psoriasis with 87% accuracy-using just nail photos and joint scans. Oral drugs like upadacitinib (expected 2024) could replace injections for many. And personalized medicine based on genetics? That’s coming by 2028.
You’re not alone. Over 1 million Americans live with this. And with the right care, you can keep moving, keep living, and keep your skin clear-not just for now, but for years to come.
Can psoriatic arthritis happen without skin psoriasis?
Yes, but it’s rare. About 15% of people develop joint symptoms before any skin changes appear. If you have unexplained joint pain, especially with a family history of psoriasis, get checked. Skin lesions may appear later.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis usually affects joints symmetrically and often shows up in blood tests. Psoriatic arthritis is asymmetric, rarely shows positive blood markers, and always comes with skin or nail changes. Nail pitting and dactylitis are unique to psoriatic arthritis.
Do biologics cure psoriatic arthritis?
No, they don’t cure it. But they can put the disease into long-term remission. Many people stay symptom-free for years while on biologics. Stopping them often leads to flare-ups, so most stay on them long-term under doctor supervision.
Can I use over-the-counter painkillers instead of prescription meds?
NSAIDs like ibuprofen can ease pain and swelling short-term, but they don’t stop joint damage. If you rely on them alone, you risk permanent deformity. Prescription drugs like DMARDs and biologics are designed to halt progression-not just mask symptoms.
How do I know if my treatment is working?
Look for three signs: less joint swelling, clearer skin, and lower fatigue. Your doctor may also use a scoring system like MDA (minimal disease activity). If after 3-6 months you still have swollen joints or thick plaques, it’s time to adjust your treatment-not wait longer.




Pat Mun
February 12, 2026 AT 11:51