How to Communicate with Your Pharmacy During Generic Drug Transitions
February 7 2026Bioequivalence: Why It Matters for Generic Drugs and Your Health
When you pick up a generic pill, you expect it to do the same job as the brand-name version—and bioequivalence, the scientific standard that proves two drugs deliver the same amount of active ingredient at the same rate in the body. Also known as therapeutic equivalence, it’s not just a regulatory checkbox—it’s what keeps you safe when switching from expensive brands to affordable generics. Without it, a drug meant to control seizures, prevent blood clots, or manage HIV could fail—or worse, cause harm.
Some drugs don’t have room for error. narrow therapeutic index drugs, medications where the difference between a helpful dose and a dangerous one is very small, include blood thinners like warfarin, anti-seizure drugs like phenytoin, and thyroid meds like levothyroxine. For these, FDA bioequivalence, the strict testing process the U.S. Food and Drug Administration uses to approve generics is far more rigorous than for regular pills. The FDA requires generics to match the brand within a tighter range—often 90% to 111%—to make sure your body gets exactly what it needs. Skip this step, and you risk underdosing (which lets your condition flare up) or overdosing (which can cause toxicity).
It’s not just about the numbers. Bioequivalence also means the drug dissolves the same way, gets absorbed the same way, and behaves the same way in your system. That’s why a generic version of a blood pressure pill shouldn’t make you dizzy when the brand didn’t. It’s why switching from one generic to another shouldn’t trigger new side effects. And it’s why the FDA and other agencies like the EMA and Health Canada don’t just trust manufacturers—they test batches, monitor real-world reports, and require detailed studies before approval.
Some people still worry generics aren’t as good. But the truth is, most generics are just as safe and effective. The real danger isn’t the generic itself—it’s when bioequivalence isn’t enforced. That’s why posts here dig into how generic labels are required to match brand names exactly (even when that delays safety updates), why some drugs like nevirapine or primaquine need extra caution, and how timing, dosage, and even your body’s reaction can be affected by small differences in how a drug is made. You’ll find real examples: how a mismanaged bioequivalence standard could lead to treatment failure in HIV, how a generic statin might be fine for most but risky for someone with kidney issues, and why you should never assume all generics are created equal.
Whether you’re taking a daily pill for cholesterol, managing a chronic condition, or just trying to save money without sacrificing safety, understanding bioequivalence helps you ask the right questions. It’s the invisible rule that keeps your meds working—and keeps you out of the hospital. Below, you’ll find clear, practical guides that break down exactly how this system works, where it breaks down, and what you can do to stay protected.
 1 Feb
1 Feb
Dissolution Testing: How the FDA Ensures Generic Drug Quality
Dissolution testing is the FDA's key method for ensuring generic drugs release their active ingredients at the same rate as brand-name versions, replacing the need for costly human trials while guaranteeing safety and effectiveness.
Read More... 15 Jan
15 Jan
Patient Trust: How to Build Confidence in Generic Medications
Learn how to build trust in generic medications, why patients doubt them despite proven safety and effectiveness, and what doctors and pharmacists are doing to change that. Save money without sacrificing quality.
Read More... 7 Jan
7 Jan
Pharmaceutical Equivalence for Generics: What It Really Means When You Pick a Generic Drug
Pharmaceutical equivalence means generic drugs contain the same active ingredient, strength, and dosage form as brand-name drugs. Learn what it really means for safety, effectiveness, and cost savings.
Read More...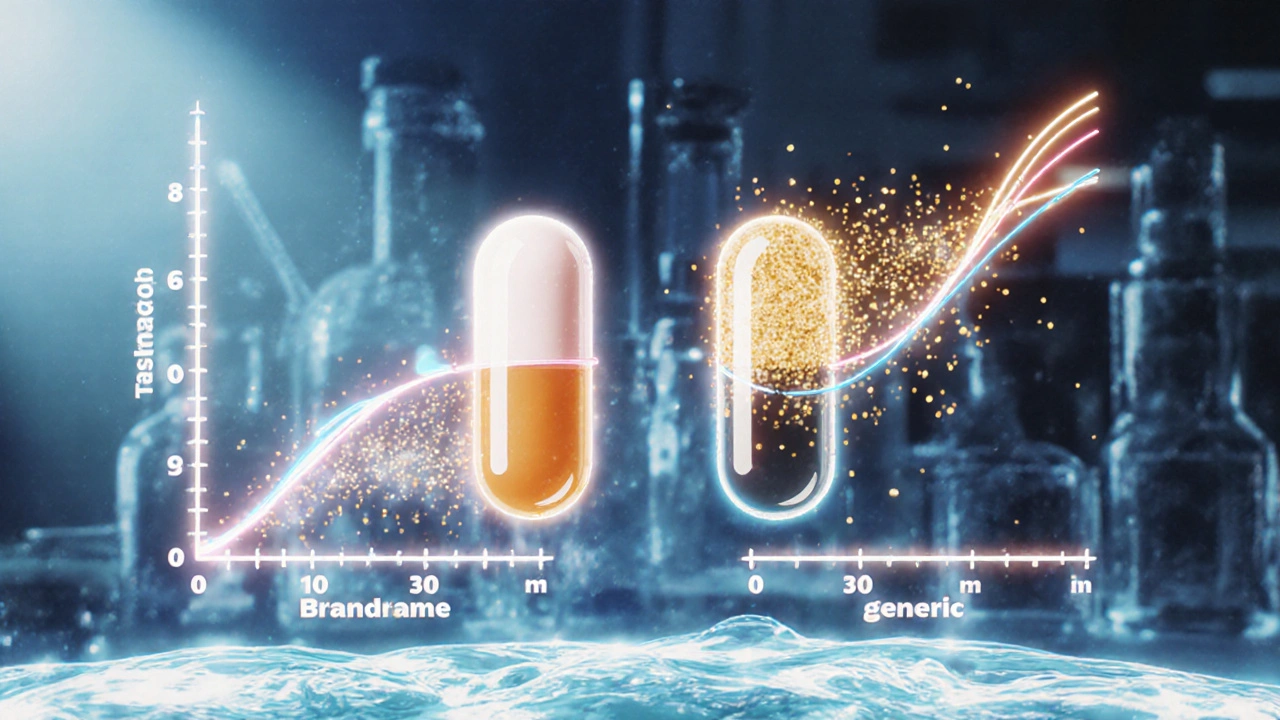 24 Nov
24 Nov
How to Compare Dissolution Profiles and What They Mean for Generic and Brand Drugs
Learn how dissolution profiles ensure generic drugs work like brand-name versions. Understand f2 similarity, regulatory standards, and why this science keeps patients safe.
Read More...




